When treating a condition such as tuberculosis (TB), doctors will often prescribe multiple weeks or even months of antibiotics. If you aren’t familiar with the side effects of long-term antibiotics, some of the most common impacts happen within the gastrointestinal tract. Diarrhea, nausea, vomiting, stomach pain, or compromised gut health are all frequently experienced side effects of these drugs.
So what can you do to keep your digestive system running smoothly, even if you are required to undergo weeks-long treatments that include antibiotics? Aiming for a balanced gut biome can be the trick to lessening side effects’ impact during long-running medication courses. Plus, it is also helpful for a multitude of conditions, from keeping your immune system robust, to improving your stress levels and clearing your skin.
What Is a Microbiome?
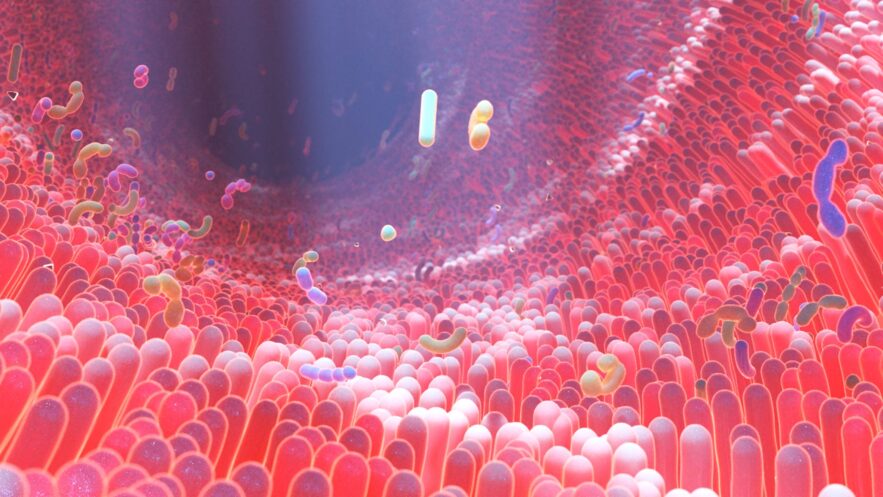
What exactly is your microbiome, anyhow?
“The human microbiome is a diverse community of trillions of microorganisms that reside in our gut,” says Alison Acerra, MS, RDN, the founder of Alison Acerra Nutrition and MedShadow Medical Advisory Board Member. “It plays a crucial role in maintaining our overall health.”
Acerra says that medications, such as antibiotics often prescribed for TB, can wreak havoc on the gut.
“The delicate balance of this microbial community, or ecosystem, can be disrupted, especially after a round of antibiotics,” she says.”Antibiotics, while essential for treating bacterial infection, can also unintentionally harm the beneficial bacteria in our gut.”
Medicines often treat all aspects of the body. There is seldom a way, especially with oral medications, to pinpoint the precise location of “attack.” An antibiotic, for example, has a job to kill bacteria. It is not able to understand that some bacteria are good for our bodies, and some bacteria are bad. It simply attacks all bacteria.
“The good news is there are steps you can take to support and restore your microbiome after completing a course of antibiotics,” says Acerra.
Why Does Your Gut Biome Matter?
Acerra says some clients ask what the microbiome even is and why they should care about protecting it.
“This is a really great question,” she says. “The microbiome is the fungi, viruses, and bacteria that live in and on our bodies. The gut microbiome in particular plays a crucial role in various aspects of our health.”
This gut biome:
- Aids in digestion
- Absorbs nutrients from consumed foods
- Supports a healthy immune system
- Helps to support maintenance of a healthy weight
- Impacts overall mood
In order to maintain balance before, during, and after a course of disruptive long-term antibiotics, which focus on killing any and all bacteria in the body, both the good and the bad, it is important to focus on diet. What you eat plays a massive role in the health and balance of your gut biome.
5 Key Steps to Nurture Your Gut Biome
There are a number of ways to stay mindful of your gut’s biome anytime. This focus is especially crucial after a course of antibiotics. The longer you’ve been on the medication, the more damage may have occurred to imbalance your biome. Here are some handy ways to restore its order.
1. Probiotics
“Probiotics are a way to introduce friendly bacteria back into the gut,” says Acerra. “When consumed in enough amounts, they help to replenish the beneficial bacteria that may have been affected by antibiotics.”
Probiotic-rich foods include:
- Yogurt
- Keifer
- Sauerkraut
- Kimchi
- Fermented foods
- Kombucha
- Tempeh
Alternatively, Acerra says, you can also find over-the-counter (OTC) supplements sold for this same purpose. She says to seek a “diverse range of bacterial strains” to support your gut health when selecting a supplement. We still have a lot to learn about exactly how probiotic supplements affect our bodies.
2. Prebiotics
Prebiotics are “fuel for your probiotics,” says Acerra.
“Prebiotics are nondigestible fibers that nourish and support the growth of beneficial bacteria in the gut,” she says.
Foods that are rich in prebiotics include:
- Garlic
- Onions
- Leeks
- Asparagus
- Whole grains
- Resistant starches such as plantains, beans, and peas.
Adding these to your diet helps to speed recovery in your gut’s biome.
3. Focus on a Fiber-Rich Diet
In what Acerra calls a “cornerstone for microbial health,” adding more fiber-focused foods helps to create a healthy microbiome.
Fiber-rich foods are technically a prebiotic, as they fuel the growth of helpful bacteria. They can include foods like:
- Whole grains
- Fruits
- Vegetables
- Legumes
- Nuts
Acerra said also that aiming for a diverse range of food can provide an adequate variety of different strains.
4. Stay Hydrated
“Hydration plays a very important role in supporting the microbiome,” says Acerra. “Water helps to transport nutrients to cells, facilitates metabolic processes in the body, and supports microorganisms in the gut.”
Many people ask “How much water do I need?” each day. Read more on water needs in MedShadow’s article here.
5. Avoid Unnecessary Long-term Antibiotics
Of course there are times, especially with a condition such as TB, when you will need long-term antibiotics. You should always discuss that need with your doctor.
“You always want to preserve the microbial balance as much as possible,” says Acerra. “Antibiotics are important for treating bacterial infections, but it is crucial to use them judiciously, and sometimes, they are overprescribed.”
Working with your healthcare professional, you can decide on the best options for your care. A comprehensive study published in December 2022 reviewed cases ranging from December 2002 to December 2017 encompassing 23 million unique patients. It found 50.9 million claims for upper respiratory infections, for which the drugs rarely provide any benefit, including sinusitis, pharyngitis, laryngitis, bronchitis and the common cold.
The odds of a patient being diagnosed with an adverse event increased 30% for those receiving antibiotics. Adverse events following antibiotics were found in as many as one in 300 prescriptions, depending on the antibiotic prescribed, or one in 1,150 prescriptions overall.”