Community pharmacists (those who work in retail pharmacies) are uniquely qualified to provide fast, accurate, and reliable medication advice. And pharmacists have long been regarded as one of the most trusted professions in America, serving as a steady anchor in communities nationwide.
In fact, Americans go to the pharmacy twice as often as they visit other healthcare providers.
But that kind of access is getting harder to find, especially in lower-income neighborhoods. This year, Rite Aid shut down all of its stores, and Walgreens plans to close one in seven stores in the next three years. CVS has shuttered more than 900 stores since 2022, with another 270 expected to close by the end of 2025.
Behind the statistics are real people, from rural towns to big cities, whose lives are affected when a pharmacy shuts its doors. It begs the question: What happens when a community loses its most accessible source of care?
‘We Need More Pharmacists in Every Neighborhood’
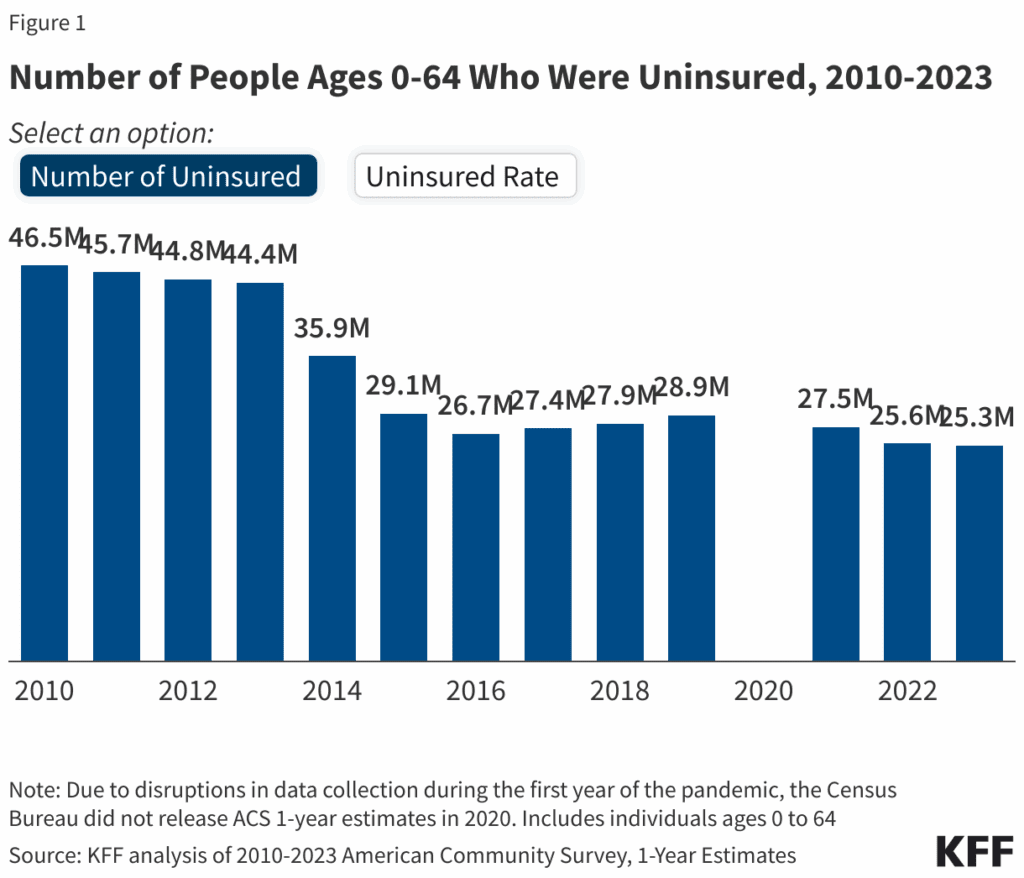
Nearly one in three Americans lack a primary care provider, and about 10% don’t have health insurance. Local pharmacists fill that gap, serving as a trusted healthcare professional who knows their name, prescription history, and often their personal story, too.
So when a neighborhood pharmacy closes, the whole community feels it. There’s the older adult who can no longer drive to pick up prescriptions. The parent searching for a child’s antibiotic after hours. And the pharmacist who’s out of work.
Local healthcare professionals see the ripple effects too. Patients skip refills, miss doses, and struggle to manage chronic conditions.
Losing the Corner Pharmacy Means Losing Easy Access to Routine Care
“Our Rite Aid used to be within walking distance of our house,” says Lindsay, 60, of San Francisco, California, who asked that her real name not be used. “My husband would stop by on his way home from work for milk and our meds. Sometimes I would walk or take the bus. We had a really solid pharmacy team there. Then we switched to Walgreens and had a good team again. But when that Walgreens closed, everything changed.”
Now, Lindsay, who has a chronic neurologic condition that limits her mobility, depends on her husband to pick up her prescriptions. She can’t walk like she used to, and even the bus is usually not an option.
It’s the kind of problem you might expect in a small town, not a major city like San Francisco. But pharmacy closures are reaching urban neighborhoods, too. In the past decade, Lindsay says she’s seen five pharmacies close near her home. Since she depends on her husband to pick up prescriptions, he has to coordinate around his work schedule. Lindsay often feels uncertainty about getting her prescriptions on time.
Receiving prescriptions by mail isn’t a simple solution for her, either. “Mail order delivery isn’t practical when you need something right away,” Lindsay says.
Lindsay says she’s also noticed the pharmacies that remain are busier, and the pharmacy staff is overworked. “We need more pharmacists in every neighborhood,” she says. “If you want healthy populations, you have to have accessible pharmacies.”
We need more pharmacists in every neighborhood. If you want healthy populations, you have to have accessible pharmacies.
One of the most devastating effects of the pharmacy closures? The loss of a relationship with a pharmacist she trusted. “That makes a big difference,” she says. “The staff knew us personally, and any issues were handled quickly.”
Lindsay doesn’t technically live in a pharmacy desert. But her experience reveals how closures ripple beyond the neighborhoods you’d expect. Traditionally, pharmacy deserts have been defined as low-income areas with no pharmacy within 1 mile in cities or 10 miles in rural areas. A low-income area is typically one where 20% or more of residents are below the federal poverty level or where the median household income is less than 80% of that of the nearest metropolitan area.
For people with limited mobility — those who can’t easily walk, drive, or pick up their own medications — each closed pharmacy can mean another barrier to basic care.
A Provider’s Perspective on Pharmacy Closures
In Del Norte, Colorado, a town of roughly 1,500, nurse practitioner Emily Boyd says residents have gone without a local pharmacy since the town’s only drugstore shut down more than two decades ago.
“Now, the closest pharmacy is 10 to 15 miles away, and the nearest pharmacy with extended and weekend hours is about 30 miles away,” she says.
That distance matters. When it’s time for a refill, the inconvenience of traveling may prevent some people from picking up their prescription on time. And adults who don’t drive, or don’t own cars, face an even bigger barrier to refilling their medications on time, Boyd notes. She says that mail-order services help some patients but not all, because it only works if the refill request is sent in early enough. Otherwise, patients risk running out of medication before the refill arrives.
For 20 years, Boyd says, no one in town has filled the role their old pharmacist once did; someone who truly looked out for residents. “The pharmacist was like a second doctor, in a way,” Boyd says. “He worked closely with local clinics, and was the one having face-to-face conversations with patients,” she adds.
The pharmacist was like a second doctor, in a way. He worked closely with local clinics, and was the one having face-to-face conversations with patients.
Boyd also notes that people in Del Norte sometimes go to the emergency room for health issues that aren’t truly urgent, because they don’t have anywhere else to go. When clinics are closed and there’s no pharmacy in town, the ER can feel like the only option.
This issue isn’t unique to Del Norte. A lack of pharmacy access can contribute to missed medication doses for a variety of conditions, which increases hospitalizations and ER visits, especially among older adults.
Why Easy Access To Pharmacies Is Essential
A 2025 study found that nearly one in five Americans lives in a pharmacy desert, and another 9% have easy access to only a single pharmacy, with people living in small, rural communities most at risk for lack of access. In that study, a pharmacy desert was defined as an area where it takes longer to reach the nearest pharmacy than it does to reach a grocery store.
Some of the benefits of pharmacies are obvious, but others often go unnoticed. Here are a few ways local pharmacists and pharmacy staff support their community:
- They ensure medication safety. Effective interactions between pharmacists and patients improve medication adherence, prevent medication errors, and support better health outcomes.
- They’re easy to engage with. You don’t need an appointment to walk into a pharmacy or ask your pharmacist a question. That accessibility matters, especially with nearly 75 million Americans lacking easy access to a primary care clinic, and an expected physician shortage of nearly 90,000 physicians by 2037.
- They work when others don’t. Many pharmacies stay open later than primary care clinics and some are open 24 hours a day.
- They increase vaccination access. More than 60% of adult flu shots, and nearly 90% of Covid-19 vaccines, were given at a pharmacy in the 2024 to 2025 flu season. And pharmacists have also been shown to increase public trust in vaccines.
- They help prevent unnecessary ER visits. In one Canadian study of nearly 5,000 walk-in consultations at community pharmacies, pharmacists successfully managed most minor health concerns, referring only about 15% of patients to other providers. In follow-up interviews, about one in five patients said the pharmacist helped them avoid an ER trip.
- They improve chronic condition management. Pharmacists have been shown to improve patient outcomes in several chronic conditions, including diabetes, high blood pressure, and asthma.
- They reduce health disparities. Community pharmacists provide medication access, effective communication, and patient education in underserved areas, helping reduce inequities in care.
Finding Solutions: How We Can Protect Access To Care
Several factors are driving the current wave of pharmacy closures. Declining in-store sales and foot traffic, the rise of online shopping, and staffing issues are just a few reasons. Pharmacy benefit manager (PBM) practices, which are third-party companies that manage prescription drug benefits for insurers and employers, may also contribute significantly to closures by driving patients to use insurer-affiliated online pharmacies such as OptumRx or Express Scripts, which are owned by the PBM or its parent company. This is especially true for independent pharmacies, which are disproportionately affected by PBMs.
The American Medical Association has called for more regulatory oversight of PBMs. Meanwhile, to protect access, local, state, and federal efforts are underway to help existing pharmacies stay in business and encourage new ones to open where they’re needed most. Proposed or ongoing solutions include:
- Increasing prescription reimbursement rates for pharmacies, especially those serving Medicare and Medicaid patients
- Offering supplemental dispensing fees, which are extra payments to pharmacies meant to offset high operating costs in underserved areas.
- Providing grants or tax benefits for pharmacies that serve several neighborhoods, or that are in areas where access to pharmacies is low
In areas where pharmacies have closed, increasing access through transportation vouchers, home-delivery of medications, and telepharmacy services may help. However, these practices can cause delays in therapy, reduce interaction time with pharmacists, and come with additional fees. And for many people, these services don’t compare to talking with their pharmacy staff face-to-face.
What To Do If Your Pharmacy Closes
Pharmacy closures can be stressful, especially if you take medications regularly or you live in an area with limited options. But taking a few proactive steps can help keep you connected to care and avoid missed doses, even if you don’t have another pharmacy nearby:
- Find out where your prescriptions are being transferred. Ask your current pharmacy where your prescriptions will go before they close. If your pharmacy has already closed, call the phone number on your prescription label. It may connect you to the new location automatically. If your pharmacy is already closed and you can’t find out where your prescriptions went, contact your prescriber to send new prescriptions to your chosen pharmacy.
- Ask for a 90-day supply. If you take medications for chronic conditions, ask your prescriber whether you can receive a 90-day supply to reduce the risk of running out during your pharmacy transition. Not all insurance plans cover 90-day fills for maintenance medications, but it’s worth checking with your plan.
- Weigh your options. If you have an independent pharmacy in your area, consider asking for your prescriptions to be transferred there. Independent pharmacies often provide more personalized service and may be more flexible in offering home delivery.
- Learn your delivery or transportation options. Does your new pharmacy have home delivery, curbside pickup, or mail order? Learn what your options are, but keep in mind that mail-order may not be ideal for medications you need the same day. If getting to a pharmacy is a challenge, ask your community health center about transportation assistance options in the area.
- Keep your healthcare team in the loop. Tell your prescriber and clinic about your pharmacy’s closure. They can help suggest local options or connect you to delivery services. Once you choose a new pharmacy, let your prescriber know so they can send future prescriptions to the right place.
- Keep a medication list. Maintain an up-to-date list of your medications and their dosages. You can ask your pharmacy for a printed record of the medications you’ve filled in the past year and compare it to what you currently take. Include any over-the-counter products and supplements. Share the list with your new pharmacy to make sure nothing is missed during the transition.
If your pharmacy closes, you still have options. Even if another pharmacy isn’t just around the corner, knowing what resources exist in your community can help you get the care you and your family needs.





