
5 Common Meds That Cause Liver Damage
Your liver is one of the body's most crucial organs. Unfortunately, many drugs can put extra strain on it. Find out which ones do and how to minimize harm.
Share
Gina Jansheski, M.D., is a pediatrician with 22 years of practice experience. Dr. Jansheski completed her medical education at the University of Arizona College of Medicine, followed by a pediatric residency and a one-year fellowship in Developmental and Behavioral Pediatrics. She served as the medical director of Tucson Pediatric Hospitalists, providing pediatric hospice and palliative care services.
on this page:
Your liver is one of your body’s most crucial organs. Unfortunately, many drugs can put extra strain on it. Find out which ones do and how to minimize harm.
Day in and day out, week after week and year after year, as you eat, drink and take medications or supplements, there’s an unsung hero working hard to filter and process all of these substances, store the nutrients and get rid of the waste: your liver. That adds up to lots of chances that something passing through might harm this vital organ.1 Numerous medications, for example, have been shown to increase the risk of liver damage – that goes for herbal medicines, too, as well as dietary supplements.
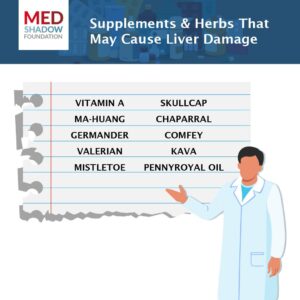
“There is increasing evidence that complementary and alternative medicines such as supplements and herbs can cause liver damage. These include kava, comfrey, mistletoe and others,” says Lauren Aleksunes, PharmD, PhD, associate professor of pharmacology and toxicology at the Ernest Mario School of Pharmacy at Rutgers University and resident scientist at the Environmental and Occupational Health Sciences Institute. “Just because they can be purchased without a prescription does not mean they are safe.”
Stay Informed. Sign up for our newsletters.
Independent, science-based journalism delivered directly to your inbox.
For more information on supplements that might cause liver damage, read this article: 15 Supplement Ingredients to Always Avoid.
According to the Centers for Disease Prevention and Control (CDC), 4.5 million adults in the U.S. are diagnosed with chronic liver disease.2 Liver disease from drugs is uncommon overall, so don’t panic if you see a medication you use on the list below. Ask your doctor if your liver function needs to be checked. And, as with all drugs and supplements, make sure you are taking the lowest effective dose for the shortest period of time.
The following five over-the-counter (OTC) and prescription drugs are some of the most common medications known to cause liver damage, according to Norman P. Tomaka, MS, FAPhA, a consultant pharmacist and health care risk manager based in Melbourne, Florida, and media liaison for the American Pharmacists Association.
1. Tylenol (acetaminophen)

A common remedy for mild pain and fever, acetaminophen can damage your liver if you take too large of a dose, either accidentally in overdose or with overuse.3
Acetaminophen is known to cause liver damage by producing a toxic metabolite in the body that accumulates over time and causes a change in the structure of the liver, which lowers its ability to perform its regular functions.
Overdosing by mistake is easily possible with acetaminophen, either when taking it alone or combined with other common OTC medications. In general, most adults can safely take between 650 mg and 1,000 mg of acetaminophen every 4 to 6 hours up to a maximum of 3,000 mg in a 24-hour period. Be aware of combination products that contain acetaminophen, and read the labels of all drugs you take to make sure you are not taking more than one medicine that contains this drug. These include commonly used OTC cough, cold and pain medications. Labels may not list acetaminophen as an ingredient, but instead, they might use abbreviations like APAP, AC, acetaminophen, acetaminoph, acetaminop, acetamin or acetam.4
Tylenol can also cause damage to the liver when taken with alcohol.4 For more on Tylenol overdose risk, read Acetaminophen (Tylenol and Generics) is Too Easy to Overdose On.
Other pain medicines that are commonly associated with liver injury include Advil (ibuprofen), Voltaren (diclofenac), and sulindac.5,6,7
2. Zyloprim (Allopurinol)
This medicine is commonly used to treat gout and is sometimes taken to prevent recurring kidney stones. It most commonly causes liver damage by provoking an allergic response in the body.8
3. Amoxicillin/Clavulanate
This medication is a combination of an antibiotic and a drug that prevents bacteria from destroying the antibiotic. It is used to treat bacterial infections, including pneumonia, urinary tract infections and sinusitis. It is also believed to cause liver damage in certain individuals by triggering an allergic response in the body, but researchers have not yet figured out the exact process by which this happens.9
Other antibiotic and antifungal medicines commonly associated with liver injury include isoniazid, trimethoprim/sulfamethoxazole, erythromycin, nitrofurantoin, minocycline, and ketoconazole.10, 11, 12, 13, 14, 15
4. Lipitor (Atorvastatin)
Statins, which are used to reduce cholesterol and triglyceride levels, can potentially harm the liver, although this is uncommon.16 Atorvastatin is thought to cause liver damage by producing a toxic metabolite or provoking an allergic reaction, although the exact mechanism is unknown.
Zocor (simvastatin), another statin drug, has also been associated with liver injury.
Aleksunes adds that liver damage from these medications, when it does occur, is usually mild and typically reversible after the patient stops taking the drug (with guidance from their health care provider, of course).
5. Depakote (Valproate)
This medication is used to prevent some types of seizures in patients who have epilepsy. It is also used in the treatment of bipolar disorder and to prevent migraine headaches. It can directly cause liver damage by causing fat deposits within liver cells – a condition known as steatosis – and inflammation, which reduce the liver’s ability to carry out its normal functions.17
Other anticonvulsants that have been associated with liver damage in some patients include Tegretol (carbamazepine) and Dilantin (phenytoin). 18, 19
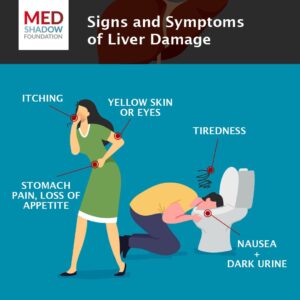
Look for signs and symptoms of liver damage if you are taking one of these medications. These usually appear within six weeks of starting a drug and may include abdominal pain, nausea, tiredness, dark urine, loss of appetite, itching, and yellow skin or eyes.19 Stop taking the medication and contact your prescriber immediately if you observe these symptoms.
In addition to medicines and supplements, “it is becoming increasingly evident that differences in a person’s genetics can heighten the risk of liver damage,” according to Aleksunes. To help you avoid these side effects, she suggests you talk to your pharmacist and health care providers about any herbal and supplement medications you are taking, as some OTC supplements can lead to liver damage. Also, read the drug insert that you receive from the pharmacist, which will let you know if the prescribed medication has the potential to cause liver damage.
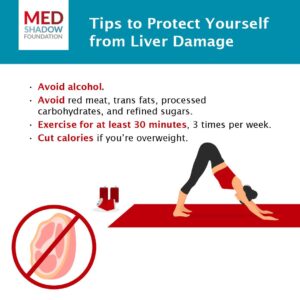
Tomaka also emphasizes the importance of taking your medicine as directed on the label or prescription. This is critical for OTC medicines that you might not suspect could cause a problem. Never take a double dose at one time, and do not exceed the maximum daily dose noted on the label.
This article was originally published on October 14, 2020. It was updated with new research by Emma Yasinski on July 25, 2024.
- Viral Hepatitis Basics. (2024, July 30). CDC.Chronic Liver Disease and Cirrhosis. (n.d.). CDC.
- Acetaminophen. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Acetaminophen. (n.d.). MedlinePlus.
- Ibuprofen. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Diclofenac. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Sulindac. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Allopurinol. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Amoxicillin-Clavulanate. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Isoniazid. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Sulfamethoxazole-Trimethoprim. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Erythromycin. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Nitrofurantoin. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Minocycline. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Ketoconazole. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Averbukh, L. D., Turshudzhyan, A., Wu, D. C., & Wu, G. Y. (2022). Statin-induced Liver Injury Patterns: A Clinical Review. Journal of Clinical and Translational Hepatology, 10(3), 543–552.
- Valproate. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Carbamazepine. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Phenytoin. (2012). [LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]]. National Institute of Diabetes and Digestive and Kidney Diseases.
- Symptoms & Causes of Cirrhosis. (2023, September 6). National Institute of Diabetes and Digestive and Kidney Diseases.
DISCLAIMER: MedShadow provides information and resources related to medications, their effects, and potential side effects. However, it is important to note that we are not a substitute for professional medical advice, diagnosis, or treatment. The content on our site is intended for educational and informational purposes only. Individuals dealing with medical conditions or symptoms should seek guidance from a licensed healthcare professional, such as a physician or pharmacist, who can provide personalized medical advice tailored to their specific circumstances.
While we strive to ensure the accuracy and reliability of the information presented on MedShadow, we cannot guarantee its completeness or suitability for any particular individual’s medical needs. Therefore, we strongly encourage users to consult with qualified healthcare professionals regarding any health-related concerns or decisions. By accessing and using MedShadow, you acknowledge and agree that the information provided on the site is not a substitute for professional medical advice and that you should always consult with a qualified healthcare provider for any medical concerns.
on this page:
RECOMMENDED:
DONATE:
Help fund our fight for improved medication safety and transparency by supporting our independent journalism.
Give NowStay Informed. Sign up for our newsletters.
Independent, science-based journalism delivered directly to your inbox.
About Our Advocacy:
We seek to create a world where there are safer medications for all and where all people are fully informed about their medication benefits and side effects, using our explanatory and investigative journalism to both inform and stimulate public discussion to drive toward solutions.
WEBINARS
Want to hear expert insights about medication safety and other care options? Watch all our past webinars and sign up for upcoming ones.
WATCH Now


