This month, we celebrate what makes Hispanic heritage wonderful and unique. We’d like to bring up another way to acknowledge Hispanic Heritage Month: learning how to manage the Hispanic health and healthcare challenges unique to your genetic background.
As Americans strive to remember that “all men are created equal,” no matter our age, skin color, religion, sexuality, gender, or socio-economic status, but research shows different ethnic backgrounds face higher or lower risks of experiencing certain health conditions. s Knowing the risks associated with your ethnicity can help you make educated decisions about your health.
Let’s break down some of the health challenges that members of the Hispanic racial or ethnic group may encounter more often than people of other heritages.
A Deep History
According to the Library of Congress, Americans “observe National Hispanic Heritage Month from Sept. 15 to Oct. 15 by celebrating the histories, cultures and contributions of American citizens whose ancestors came from Spain, Mexico, the Caribbean, and Central and South America.”
With such varied backgrounds, there are many factors that alter the health concerns of each nation. From the environment of our ancestors, to the traditional foods we historically enjoy, our past does seem to have a way to catch up to us.
With an observation that began in 1968 with the adoption of Hispanic Heritage Week under President Lyndon Johnson, the celebratory event was expanded by President Ronald Reagan in 1988. Hispanic Heritage Month now consists of a 30-day period from mid-September to mid-October.
It may seem strange to some that the date begins in the middle of a calendar month, but it shouldn’t. Sept. 15 is significant because it is the anniversary of independence for Latin American countries such as Costa Rica, El Salvador, Guatemala, Honduras, and Nicaragua.
Additionally, Mexico and Chile celebrate independence days on Sept. 16 and Sept. 18, respectively. Also, Columbus Day or Día de la Raza, which is October 12, falls within this same 30-day period.
Within the unique month, there are many significant dates that the Hispanic communities celebrate, marking it an ideal time to observe the contributions and cultural impacts so many have contributed to today’s society.
A Different Experience for Hispanics
Our genes are not the only things that determine our health risks. Society has a big impact as well.
Access to Health Insurance and Care
If you don’t have access to healthcare, you’ll be less likely to catch illness early and get treatment before it progresses. According to the PEW Research Center, Hispanics are less likely than any other group of Americans to have health coverage.
“Language and cultural barriers, as well as factors such as higher levels of poverty, particularly among recent Hispanic immigrants, are among the social and economic dynamics that contribute to disparate health outcomes for Hispanic Americans,” said the PEW Research Center’s review of the culture’s experience with health insurance.
According to the Department of Health and Human Services, Hispanics have the highest uninsured rates of any racial or ethnic group within the United States.
“In 2020, the Census Bureau reported that 49.9 % of Hispanics had private insurance coverage, as compared to 73.9 % for non-Hispanic whites,” said the HHS. “In 2020, 35.9 % of all Hispanics had Medicaid or public health insurance coverage, as compared to 33.8 % for non-Hispanic whites.”
Still more Hispanics have no health care coverage at all.
“Those without health insurance coverage varied among Hispanic subgroups: 20.3 % of Mexicans, 8.0 % of Puerto Ricans, 14.0 % of Cubans and 19.4 % of Central Americans. In 2020, 18.3 % of the Hispanic population was not covered by health insurance, as compared to 5.4 % of the non-Hispanic white population per Census Bureau report.”
These massive discrepancies became even more apparent when COVID-19 took the world by storm.
“Hispanic Americans are far more likely than White Americans to have been hospitalized or died because of the coronavirus,” said the PEW Research Center.
It’s not just insurance. Several other obstacles can make it more difficult for Hispanic Americans to get the healthcare they need. “Language and cultural barriers, as well as factors such as higher levels of poverty, particularly among recent Hispanic immigrants, are among the social and economic dynamics that contribute to disparate health outcomes for Hispanic Americans,” said the PEW Research Center’s review of the culture’s experience with health insurance.
More Dangerous Jobs
In addition to access to healthcare, there are other factors the Hispanic communities have identified themselves for a different medical outlook on life.
According to the PEW Research, Hispanics noted that their jobs have a lot to do with health risks.
“The Center survey asked people for their beliefs about the factors behind health disparities for Hispanic people,” explained PEW. “Hispanic Americans cite working in occupations with health risks as the top factor for why Hispanic people generally have worse health outcomes than other U.S. adults.”
Overall, 53% say that “working jobs that put them at risk for health problems” is a major reason for health disparities among Hispanic people in the U.S. Other major contributions to different health outcomes, as cited by the research, included language barriers, access to quality healthcare providers, immigration status, biased treatment at medical facilities, and lower income.
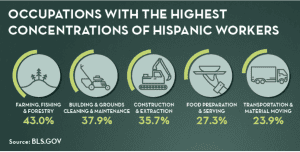
The Department of Labor notes that Hispanics offer the highest concentration of workers in positions such as those in farming, landscaping, construction, food service, and moving. These roles require more physical labor and create a higher risk of injury.
Not surprisingly, the most injuries are reported, according to OSHA, in the top ten fields of:
- Fishing and Hunting
- Logging
- Roofers
- Construction
- Pilots
- Trash hauling
- Metal Workers
- Delivery and Truck Drivers
- Mining
- Farming
Of these top ten, five are also those that have the highest concentration of Hispanic workers.
Place of Birth
The Centers for Disease Control (CDC) notes that another major factor in determining healthy outcomes for the Hispanic population include where they were born. Those born within the United States are more likely to have quality health care, as well as more frequent visits.
According to the CDC, compared with US-born Hispanics, foreign-born Hispanics have:
- About half as much heart disease;
- 48% less cancer;
- 29% less high blood pressure;
- 45% more high total cholesterol.
Additionally, the studies from the CDC note that “cancers related to infections (cervical, stomach, and liver) are more common among Hispanics born in another country.”
Social Impacts
The CDC echoed the impacts discussed by PEW’s research, noting that there were several societal factors that weighed on the Hispanic community. Some of the most astounding figures the CDC noted included the following.
“Social factors may play a major role in Hispanic health,” said the report.
Among Hispanics living in the US:
- About 1 in 3 has not completed high school;
- About 1 in 4 lives below the poverty line;
- About 1 in 3 does not speak English well.
These issues weigh heavily on access to quality healthcare, which of course, in turn, weigh on the overall health conditions of the Hispanic community.
A Difference in Outcomes
As a result of both social and genetic factors, Hispanic Americans experience different health outcomes than those of other ethnicities.
A Longer Life Expectancy
Let’s start with a positive. According to the Kaiser Family Foundation, one major benefit to being Hispanic is a longer life expectancy.
“Provisional data from 2020 show that overall life expectancy across all racial/ethnic groups was 77.3 years,” said the KFF study. “Life expectancy for Black people was only 71.8 years, compared to 77.6 years for White people, and 78.8 years for Hispanic people.”
KFF noted, however, that the COVID-19 pandemic lowered the life expectancy among all groups, and disproportionately impacted the Hispanic and Black populations
“Overall life expectancy declined by 1.5 years in 2020, with larger decreases for the Hispanic (3.0 years) and Black (2.9 years) population, compared to the White population (1.2 years), largely reflecting the disproportionate impacts of COVID-19 for these groups.”
Common Health Disparities
Even if access to healthcare were equal, studies suggest that Hispanics would experience chronic illness at higher rates than their white counterparts.
“Non-communicable diseases including type 2 diabetes mellitus, coronary heart disease, hepatic steatosis, and cancer are more prevalent in minority groups including Hispanics when compared to Non-Hispanic Whites, leading to the well-recognized terminology of health disparities,” said a study in the National Library of Medicine.
Genetics still represent a major factor when weighing risk factors for contracting certain conditions.
NLM studies show the Hispanic population is more likely to experience difficulties with:
- Obesity
- Type 2 Diabetes
- Heart Disease
- Non-Alcoholic Fatty Liver Disease (NAFLD)
- Cancer
than other ethnic groups.
Northwestern Medicine noted that a few other chronic conditions were frequently found in Hispanic persons, including:
- Hypertension (high blood pressure)
- Chronic kidney disease
- Chronic liver disease
Lifestyle
The health status of all persons is not equal. From access to care, to genetic dispositions, there are plenty of variants that can impact Hispanic health.
Even among those of Hispanic descent, there are discrepancies among different cultures. The CDC said that lifestyle factors vary among those that identify as Latino. These changes make an impact on measures to improve Hispanic health.
“Health risk can vary by Hispanic subgroup—for example, 66% more Puerto Ricans smoke than Mexicans,” said the CDC. This means that those of Puerto Rican origin may be more likely to suffer lung-related illness than those of Mexican origin.
Hispanic Disease Control and Prevention
The good news is, there’s a lot that you can do to mitigate your healthcare risks. With added knowledge, preventive care, and awareness of these disparities, Hispanics can be proactive in their personal medical care.
Focusing on these conditions can help you not only keep a mindful eye on your own health, but also direct your community health workers.
Obesity
According to Northwestern Medicine, “Hispanic Americans are 1.2 times as likely to be obese than non-Hispanic whites. This is especially important because obesity can lead to other health challenges.”
There are many risk factors for obesity, ranging from diet and activity levels to genetics and exposure to endocrine-disrupting chemicals, but the National Library of Medicine notes that obesity is especially high among Hispanic children and adolescents.
Obesity raises your risk for many other conditions.
“It is also common knowledge that obesity plays a major role in the development of type 2 diabetes and heart disease,” said the NLM report.
Luckily, other studies note that while genetics is one of many significant risk factors, it is not an inevitable outcome.
The Hispanic Community Health Study/Health Study of Latinos (HCHS/Sol) reported that other environmental factors had a bigger impact than genetics.
The HCHS/Sol study reported that “a 42.9% prevalence of obesity in Hispanic women and 36.6% in Hispanic men with extreme obesity in 7.3% of women and 3.5% in men” was notable in Hispanic adults living in the United States. In short, many living in the U.S. tend to be heavier than their counterparts in other countries throughout the world.
That said, the time they had lived in the country changed statistics, as well.
“Interestingly, the longer time living in the United States was strongly correlated with obesity in Hispanics, indicating that a longer time exposed to social and environmental factors influences behavior and risk of obesity,” said the HCHS/Sol study. “In this study, acculturation was not associated with obesity.”
Chronic Liver Disease
Hispanic people have a higher rate of chronic liver disease. Obesity is a risk factor for the condition, but not the only one.
Northwestern Medicine says that this is a major risk factor when it comes to liver disease in Hispanic patients.
“Hispanics are at higher risk for developing certain liver diseases,” said the study. “Although the exact cause is unknown, it can be a result of conditions such as chronic alcoholism, obesity, and exposure to hepatitis B and C viruses.”
Whether cultural or genetic, Hispanic health is certainly impacted by the illness. Disease control measures can include losing weight, decreasing your alcohol consumption, and monitoring your overall health issues.
In some suffering from chronic liver disease, a change in diet can help. The NLM noted that the genetics that often make-up those in the Hispanic cultures, also are known to respond well to n-3 fatty acids.
“Due to the American Indian and African ancestry in Latinos, they might also benefit by higher intake of n-3 fatty acids to alleviate NAFLD and the inflammatory-related diseases,” said the NLM.
Diabetes
Type 2 Diabetes is another condition that Hispanics experience more often when compared to their same-age counterparts.
“About 40% of adults in the United States are expected to develop type 2 diabetes in their lifetime,” reported Northwestern Medicine. “However, more than 50% of Hispanics are expected to someday be diagnosed with it.”
One Circulation Research study noted that “Hispanic adults have 80%, and children have five-fold, higher rates than non-Hispanic whites (NHW).”
The NLM also noted that it isn’t just the social factors, such as lower income resulting in a poorer diet, that make the impact. A study of Hispanic genetics shows they also have higher rate of impaired glucose tolerance.
“Hispanics are more insulin resistant than NHW (20.2% versus 15.3%),” said the study.
As a result of these factors, the illness becomes one of the conditions most likely to cause death in Hispanics.
“Hispanics are about 50% more likely to die from diabetes or liver disease than whites,” said the CDC.
High Blood Pressure
Another key factor in disease control includes monitoring one’s high blood pressure. Northwestern Medicine studies show that this condition is another that is far more prevalent in the Hispanic community.
“Nearly 1 in 4 Hispanics has high blood pressure, which can be a precursor to a heart attack, stroke, kidney disease or heart failure,” said Northwestern Medicine.
Because high blood pressure can lead to high risk factors in several other conditions, it is an important level to monitor in Hispanic patients. Poorly controlled high blood pressure among Hispanics is what the CDC labels as a “chronic disease burden.” Among Hispanics, the frequency of hypertension is 68%, compared to the 54% rate that is seen in non Hispanic whites.
Controlling elevated blood pressure is one of the most important things you can do to reduce your risk of other illnesses.
Cancer
The leading cause of death, according to the CDC, in NHW is heart disease. And, while this still ranks at a concerning number two among Hispanic populations, there is one illness that tops it.
Hispanics are most likely to die from cancer. In NHW, this is a second leading cause of death. Why the flip-flop?
Again, there is not one simple answer, but studies show that Hispanics are 28% less likely than white counterparts to receive colorectal screening, meaning that colorectal cancer rates increase.
And again, where a person is born seems to weigh on cancer-related statistics. U.S. born Hispanics can often have a different rate than foreign born Hispanics.
“Cancers related to infections (cervical, stomach, and liver) are more common among Hispanics born in another country,” said the CDC.
The NLM echoed these findings.
“Evidence has also shown that the unequal burden in disease among minority populations can be partially explained by genetic background,” said the NLM. “When compared to NHW, Hispanics have a lower incidence rate of breast cancer, prostate, and lung cancer; however, they present more of those cancers that are associated with infection.”
The NLM also made note that it was not simply the types of cancers that varied, but the stage of the illness, as well.
“Hispanics tend to have a cancer diagnosis at an advanced stage compared to NHW due to lower access to medical care, lower socioeconomic status, and proper screening,” said the study.
The NLM study also noted that far more research needs to be done with Hispanic groups.
“There are still many unknown factors regarding cancer risk in Hispanics,” said the NLM. “More information is needed regarding the proportion of genetic ancestry in diverse Hispanic populations and how this relates to cancer prevalence.”
How Do Hispanics Improve Overall Health?
Clearly, there are plenty of health indicators that all Hispanics can benefit from monitoring closely. Keeping a healthy weight, receiving quality healthcare, including yearly visits to a primary care provider, and lowering behavioral risk factors can all add to a healthier lifestyle.
While there are genetic health disparities among Hispanics as compared to NHW counterparts, there is still plenty that can be done among all racial and ethnic groups.
From the Government
The federal government has made several programs to combat the health disparities among Hispanic populations. Some of the attempts to balance the scales have included:
- Additional access to insurance with the Affordable Care Act
- Providing educational resources for community health workers
- Monitoring health trends with research
Additionally, programs to assist all persons with lower income to improve their quality of life can also contribute to improving health issues. Health care costs are not the only impact when it comes to lower socio-economic status.
“There are numerous factors that impact health disparities in the described chronic diseases. Low socioeconomic status, with the associated poverty and low education level, in addition to not having appropriate access to health care and early diagnosis, contribute to the severity of the disease and to the increased mortality,” said the NLM study’s conclusions.
What You Can Do
To balance health equity on your own, you can take a personal approach to handling your own (and family and friends) medical care and being an advocate for your wellness. To do so, remember to:
- Obtain health insurance, via employers or the Affordable Care Act
- Maintain a primary care physician and schedule annual wellness check-ups
- Pre-screen for potential disease, including diabetes and cancers that your heritage may make you more prone to overall
- Make lifestyle improvements, such as eating a healthy diet, quit smoking, and adding exercise to your daily routines
While there are genetic issues that hinder many people in many ways, that does not mean you are helpless in fighting disease.
“An analysis of the gene variants in Latinos explains in part the increased risk for specific diseases including type 2 diabetes, CHD, and NAFLD,” said the NLM study. But being mindful of these predispositions can help you and your health care provider keep an eye on your overall health status and take into account these risk factors.






