It is difficult to know what medicine you can take while breastfeeding. Studies tend to be lacking. Advice can be confusing. Let’s dive into medication while breastfeeding.
Two years ago, a researcher who specializes in the safety of breast milk was in the midst of breastfeeding her own child when she experienced a serious bout of postpartum depression. She had a televisit with her doctor, who refused to write her a prescription for antidepressant medications as long as she was still breastfeeding, even though the drugs are often considered safe to take during pregnancy and breastfeeding.
“A lot of times, [the] health [of the new mother] isn’t prioritized as much as that of the infant. And that’s something that we really worry about,” says Kaytlin Krutsch, PharmD, a pharmacotherapy specialist with the InfantRisk Center at Texas Tech University Health Sciences Center, a group of researchers that studies the effects of drugs and supplements on breast milk. The center also provides resources for parents.
It’s not just the doctors who are cautious.
“Moms are really afraid, sometimes [of] even taking their antibiotics,” she explains. “Gosh, that’s so sad to me because it’s good for them. It’s fairly safe for the infant. And I can’t imagine just choosing to be sick and to deal with it. There’s a lot of literature out there that says that moms feel like they need to be a good mother, and to do that, they have to sacrifice their own health.”
It’s sometimes true that neither physicians nor mothers know as much as they may like about drugs and supplements — how they enter breast milk, in what doses, and what side effects those substances can have on the babies who consume breast milk. However, over the past decade, researchers like Krutsch have been systematically studying those drugs and supplements to provide better guidance.
In addition to studying different types of drugs one by one, she and her team have compiled existing evidence on many drugs and created a ranking system that describes the relative risk of using a treatment while breastfeeding and the research strength about them. The team has developed resources for doctors, as well as an app for parents called MommyMeds, in which they can learn about the safety of drugs and supplements in breastmilk by scanning the medication’s barcode.
Krutsch says throughout her research she’s been surprised by how many treatments she’s found to be safe.
“I would have thought that the risk would be much higher with a lot of these medications,” says Krutsch. “The reality is our body does a really good job at protecting the infant. Most of [the treatments] pass through [to the breast milk] in very, very low degrees.”
How Do You Make Breast Milk?
Inside the breast, you have many tiny, hollow sacs called alveoli. Your pituitary gland in your brain releases a hormone called prolactin, which signals to those alveoli to start taking nutrients from your blood to make breastmilk.
These alveoli are organized into clusters called lobules. Those lobules are connected by a series of thin tubes called ducts. Those ducts come together behind your nipple and release breast milk when you’re lactating. Think of the lobules like small cities and the ducts like roads or tunnels. The cities make milk, which is then “transported” along the roads to the nipple.
Most of the food and drinks you consume end up in your breastmilk, ass do antibodies from your immune system that help protect your newborn from illnesses. Many of the drugs and supplements you might take while breastfeeding may also pass along to breastmilk, but the doses your newborn is exposed to during breastfeeding are typically lower than they are during pregnancy.
Benefits of Breastfeeding for Baby

“The research is very clear that there are advantages of breastfeeding,” for the baby, says Nicole Derish, MD, a psychiatrist who specializes in working with pregnant and postpartum patients. The most obvious perk is increased early immunity.
“We develop immunity over the course of life and that immunity can actually be passed through breast milk,” she says. “That is really helpful in times of infection. For example, babies that are breastfeeding, if they catch a cold, it might be a bit shorter.”
Derish adds that breastfeeding also may reduce the risk of obesity in the baby’s future.
Despite these benefits, it’s important to keep in mind that the mother’s health is also needs to be a priority. If she is unable to breastfeed or needs to supplement with formula, it’s most important that her health is protected so she can take care of herself and her baby.
Benefits of Breastfeeding for Mom
Those people who breastfeed go on to have lower risks of a variety of diseases from ovarian cancer to type 2 diabetes.
Which Drugs and Supplements Get Into Breast Milk?
Whether and how much of a substance enters your breast milk depends on two main factors: the drug’s chemistry – some are more readily absorbed than others based strictly on their makeup; and the timing of taking it.
Chemistry
Drugs and supplements all have different chemical characteristics. Some get absorbed by water and others by fats. Some bind to certain proteins in your blood, while others float freely.
These characteristics determine how and where the drugs move through your body. Drugs that are lipophilic, meaning attracted to fats, and protein-bound are more likely than others to end up in your breast milk in higher concentrations than those that aren’t, because they stick to the fats in the milk.
But, there’s more than chemistry going on. Timing also plays a big role.
Timing
Sonal Patel, MD, a pediatrician and neonatologist with a private practice specializing in helping parents and infants through the baby’s first months, explains that in the first few days after giving birth, the mother isn’t producing that much milk.
“Even if you’re using drugs that are easily passed into the milk, there’s not enough of [them] in there,” says Patel.
After about four days, she explains, the alveolar cells around the breast-milk ducts widen to allow you to pass antibodies that fight infections onto your baby. After the tenth day, post-delivery,, those cells swell up and close again, limiting the amount of drug that can be passed into the breast milk. However, at this point, moms are producing more quantities of breast milk than they were right after childbirth.
Many women who have cesarean sections (C-sections) or experience especially painful vaginal births are sometimes prescribed opioids. Patel explains that during the early days after giving birth, these drugs are unlikely to affect your infant.
After that, your physician will likely transition you to another painkiller like Tylenol or Advil, because, starting then, the opioids can get into your breast milk and dangerously slow your baby’s breathing or make it difficult for them to latch. If those drugs aren’t effective enough against your pain, it’s time to go back to the doctor for an evaluation.
“There might be something else going on that hasn’t been addressed,” says Patel.
FAQs About Medicines and Supplements While Breastfeeding
Before you decide to stop (or start) taking any medications or supplements during breastfeeding, it’s important to talk to your doctor. There are risks to taking medications during breastfeeding, but there are also risks to not treating illnesses while breastfeeding.
Derish says that if you became pregnant while using a particular treatment, it’s important to keep in mind that, “if we are concerned about exposure, and the baby has already been exposed to something, oftentimes the safest thing is to remain on that medication to avoid multiple exposures.”
She adds that, “I am a big proponent of using things that we know work [for the individual] because what sometimes happens is that we switch to a different agent thinking, ‘Oh, we have a little bit more research on this versus that,’ and we’re splitting hairs. And then maybe the mom doesn’t do as well [on a new drug]. For example, an antidepressant. Maybe we switch the mom to a different antidepressant because we have a slight amount more research on it [and its impact on baby], and they don’t do well. It doesn’t work for them. At that point, we’ve exposed the fetus to both medication and the illness.”
Here is information on some of the most commonly used medications and how they might affect your newborn.
Can I Take Mucinex or Cough Medicine While Breastfeeding?

Patel and Krutsch recommend that nursing parents limit their use of cough suppressants. These drugs, including Robitussin Cough (dextromethorphan) and Vicks 44 Cough and Cold (pseudoephedrine), can be transferred through breast milk and slow your baby’s breathing, explains Krutsch.
Patel also recommends staying away from anything containing the painkiller codeine and, again, pseudoephedrine, which is also found in Sudafed, because it can lower your milk production.
There hasn’t been much research on the main ingredient in Mucinex, guaifenesin, but experts don’t suspect it would be dangerous for newborns. Watch out for combination Mucinex drugs, which may contain alcohol or other ingredients that are unsafe for your baby.
Can I Take Ibuprofen, Tylenol, or Dayquil While Breastfeeding?
During pregnancy, Tylenol (acetaminophen) is considered safer than ibuprofen when you need a painkiller or fever suppressant, but during breastfeeding, both drugs are considered reasonably safe. [Note: there are new concerns about acetaminophen taken during pregnancy raising the risk of autism or ADHD in the infant.] Mother To Baby, an organization that studies the safety of drugs in pregnancy and breastfeeding and provides information to people and doctors, explains that the amount of each of these painkillers that makes it into your breastmilk ends up being less than the dose that a doctor would prescribe if your newborn needed one of these drugs.
However, it’s important to note that many cold and flu medications, like Dayquil, contain multiple ingredients. It’s safest to stick with a drug that contains one active ingredient, but if you do choose a combination medicine, be sure to check the label for those ingredients mentioned above like cough suppressants and other painkillers like codeine, which may not be safe for your baby.
Can I Take Antibiotics While Breastfeeding?
Some antibiotics are safer than others while breastfeeding, particularly if your newborn was born prematurely. With any antibiotic, experts recommend that you monitor your baby for diarrhea or rashes that could develop as side effects. The drugs typically do find their way into breast milk, but only in small amounts.
How Can I Prevent Mastitis While Breastfeeding?
Mastitis is a painful bacterial infection that can happen when milk gets trapped in your breast. In addition to pain, it can cause swelling and redness on the breast. It can also cause fevers. If you experience mastitis, you may be able to treat it at home, but if it’s severe, your healthcare provider may recommend that you take antibiotics. If left untreated, it could cause an abscess. Fully draining your breast while breastfeeding and varying nursing positions can help prevent mastitis, though some people are more prone to it than others.
You can discuss with your doctor if the benefits of treating mom with needed antibiotics outweighs concerns of passing medication onto the baby. While research can be limited, it is important to note that you may require medication for an infection.
Can I Drink Alcohol While Breastfeeding?

It’s well-known that alcohol is usually off-limits for pregnant people, but Patel says that it’s ok to have an occasional drink when breastfeeding. The difference, she explains, is in how that alcohol reaches your baby.
When you’re pregnant, the alcohol goes to the baby right away, but when you’re breastfeeding, the alcohol gets metabolized in your liver before it makes its way to your breast. If you’ve imbibed enough to feel intoxicated, more alcohol may make it into your breast milk so she does recommend pumping and dumping when having more than one to two drinks (pumping your breast milk out, but not giving it to your baby), before feeding your baby again.
Can I Drink Coffee While Breastfeeding?
Caffeine does pass into breast milk, but MotherToBaby suggests that it’s safe for most mothers to drink up to 300mg of caffeine per day. That’s about two small cups of coffee, though the amount of caffeine in different drinks varies widely. Check out this chart to see how much caffeine is in your favorite drinks.
If your baby seems to have trouble sleeping or is more irritable, consider reducing or cutting out caffeine while you’re breastfeeding.
Can I Take Supplements Like Ashwagandha While Breastfeeding?

You may want the benefits from some pills you take to move into your breast milk. Luckily, some important vitamins do.
“If you’re breastfeeding,” says Patel, “please, please, please take prenatal vitamins.” In addition to providing your baby with an extra boost, it’s also helping you “reestablish and rejuvenate your own nutrients,” she says.”
On the other hand, since vitamins and herbal supplements are not regulated by the Food and Drug Administration (FDA), we don’t always know how they might affect your baby. For example, there’s no evidence on how ashwagandha (withania) might affect breastfeeding infants, so the National Institute of Health (NIH) suggests avoiding that popular supplement while nursing.
Patel herself tried an herbal supplement to boost milk production while she was breastfeeding, but she noticed that it caused both her and her baby excess gas. She stopped taking it.
The app MommyMeds also offers information on the safety of many other supplements.
Can I Take Allergy Medications While Breastfeeding?
Antihistamines were once thought to reduce your supply of breast milk, but Krutsch says that’s not the case. The receptors for the drugs “just aren’t in your breasts,” she says. It’s ok to take over-the-counter allergy medicines like Benadryl, Allegra, Claritin, and Zyrtec while breastfeeding. But make sure to talk to your healthcare provider and watch your baby for changes in alertness, as some antihistamines could make your baby drowsy.
Can I Take Antidepressants While Breastfeeding?
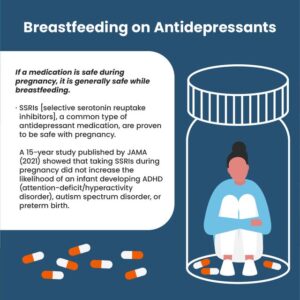
Many nursing and pregnant people, and even their doctors, worry about how psychotropic medicines might affect infants. Because of that fear, many of those drugs have been studied more frequently than others.
“SSRIs [selective serotonin reuptake inhibitors], a common type of antidepressant medicine, are over and over again proven to be safe with pregnancy,” says Patel. “And the rule of thumb is that if it’s safe in pregnancy, it’s probably safe in breast milk.” She also emphasizes the importance of remembering the physical and mental health needs of the woman doing the breastfeeding.
A 15-year study in JAMA, published this year, showed that taking SSRIs during pregnancy did not increase the likelihood of an infant developing ADHD (attention-deficit/hyperactivity disorder), autism spectrum disorder, or preterm birth. Keep reading to learn more about your options for treating postpartum depression.
Can I Take Epilepsy Drugs While Breastfeeding?
Both epilepsy and the drugs used to treat it can interfere with pregnancy, and vice versa. Pregnancy can alter the frequency of seizures, and seizures can lead to birth defects such as fetal injury and preterm birth. Anti-epileptic medications, on the other hand, can also cause birth defects such as cleft palate, neural tube defects, skeletal abnormalities, and congenital heart or urinary tract defects.
Still, many women with epilepsy conceive healthy babies. It’s crucial to evaluate the risks of the illness and medications with a healthcare provider, who might wean women off of medications if their seizures are rare, or prescribe higher doses of folic acid than pregnant women typically take to help prevent neural tube birth defects.
When it comes time to breastfeed, researchers say anti-seizure medications are not likely to harm the baby, according to a study of 223 babies born to mothers with epilepsy.
There are some cases of babies having anemia and difficulty breathing after being exposed to a common seizure medication Lamictal (lamotrigine) in breast milk, so it’s still important to monitor your baby for any changes and talk frequently with your healthcare provider. If you notice a rash or trouble breathing with the baby, stop breastfeeding.
Can I Take Antipsychotics While Breastfeeding?
In most cases, only a small number of studies have looked at pregnancy outcomes, and you and your physician will have to make decisions with the, albeit small, amount of information that is available. Researchers suspect that the risk to your infant is minimal, especially considering there is likely a significant risk to discontinuing antipsychotic medication while breastfeeding.
There is one case study of an infant being exposed to ziprasidone. That baby did not suffer any known side effects. The label of risperidone tells patients not to breastfeed while taking the drug, though a small study suggests that doses up to 6mg found in breastmilk did not cause adverse effects in babies. A few studies suggested that olanzapine is safe, but one did suggest that babies experienced mood changes and irritability after being exposed to olanzapine in breast milk.
Can I Use Retinol While Breastfeeding?
Isotretinoin is a retinoid pill that’s known to cause birth defects if taken while pregnant. However retinoids that go on your skin, such as tretinoin, are absorbed into the bloodstream in much lower quantities than pills, meaning it is far less likely to be dangerous to your infant. Still, tretinoin’s effect on breast milk hasn’t actually been studied.
Can I Take Adderall or Other ADHD Medication While Breastfeeding?
Small amounts of ritalin can make their way into your breast milk, though a small study suggests that these low doses are safe for newborns. There’s currently no information on the safety of Strattera (atomoxetine), another ADHD medication, while breastfeeding. For fact sheets on several other types of medications used to treat ADHD while breastfeeding, check out this page on MotherToBaby.
Can I Take Blood Pressure Medication While Breastfeeding?
Because preeclampsia, which is characterized by dangerously high blood pressure both during pregnancy and shortly after giving birth, it’s important if your high blood pressure cannot be controlled with diet, exercise, and stress reduction, you manage it using medications. If you have severe hypertension (blood pressure of 160 systolic blood pressure or diastolic of 110 higher) during pregnancy, your doctor may recommend one of the following three hypertensive medications, which are considered the frontline therapies for preeclampsia with severe hypertension. These drugs likely cross the placenta, meaning they can affect your fetus, but do not accumulate there, so the exposure is limited, an analysis of 30 studies found.
The three drugs are labetalol, nifedipine, and methyldopa. These same drugs are also likely to be the safest options while breastfeeding.
Can I Take Methotrexate While Breastfeeding?
In most cases, doctors do not recommend taking methotrexate, a drug commonly prescribed for autoimmune conditions such as lupus, during pregnancy or breastfeeding. There is some evidence of adverse pregnancy outcomes such as miscarriages and developmental delays for fetuses exposed to methotrexate during pregnancy. During breastfeeding, the risk is lower, but the drug does pass into breast milk. Experts recommend low doses (up to 92 mg) and monitoring your baby’s blood counts if you need to take the drug while breastfeeding.
Can I Take Humira While Breastfeeding?
Humira is a commonly-prescribed medication for a variety of conditions such as rheumatoid arthritis and digestive disorders. Small studies have shown conflicting results about whether or not the drug might harm a fetus during pregnancy, but the chances of it affecting a baby during breastfeeding appear to be low because very little amounts of the drug cross into breast milk, and it’s not easily absorbed in the baby’s digestive tract.
More Tools for Breastfeeding Safety Information
The following resources are available to check whether treatments and supplements you’re using are safe during pregnancy or breastfeeding:
- MotherToBaby
- LactMed, an NIH database
- E-lactancia, which includes both medications and supplements in English and Spanish.
- MommyMeds App, which allows you to scan products at the pharmacy and offers a risk
MedShadow Foundation’s Kimberly Bliss interviewed our friends at La Leche League to discuss other resources that can assist new and breastfeeding mothers.
When you’re at the pharmacy, you can pull up the MommyMeds app and scan any product you’re considering. It’ll give you a risk score from L1 to L5, representing how safe the treatment is for you and your baby and how confident researchers are with the level of existing evidence.
- L1 Safest: Extensive evidence demonstrating no adverse effects on the infant.
- L2 Safer: Limited evidence without an increase in adverse effects on the infant.
- L3 Probably Safe: No studies, but expert opinion suggesting safety. Risk to the infant is possible, and further evaluation must be taken to consider individual situations.
- L4 Possibly Hazardous: Positive evidence or expert opinion of risk to the infant or milk production.
- L5 Hazardous: Significant and documented risk to the infant. Contraindicated.
Postpartum Depression
Signs of Postpartum Depression
The biggest challenge in identifying postpartum depression is differentiating it from a phenomenon called “baby blues,” says Derish.
“Baby blues occur in 80% of the population, and it looks like being tearful. I always describe it as ‘you watch a fabric softener commercial and you cry, and then two minutes later, you’re fine.’”
Depression, on the other hand, is characterized by a persistent and lasting low mood. Symptoms of depression might include:
- Excess fatigue or pain (beyond what you’d expect as a new parent)
- Feeling guilt or shame
- Difficulty bonding with the baby
- Loss of joy from things that used to make you happy
- Suicidal ideation
You may be too tired or busy to participate in activities that you previously enjoyed during early parenthood, but Derish says, for example. “If you love pad thai, pad thai should still bring you joy.”
“Suicidal ideation is not uncommon, and it’s never normal,” says Derish. If you’re having thoughts of suicide, call 988, the suicide and crisis hotline.
Risk Factors for Postpartum Depression
It’s not clear how different postpartum depression is from typical clinical depression, but many women are at higher risk shortly after giving birth.
“It’s a period of increased vulnerability,” says Derish.
It’s not simple to predict who will experience postpartum depression, but there are some traits that may raise your risk, including:
- Having a history of depression
- Having had medically complicated pregnancies
- Being an adolescent
- Having limited support from family and friends
- Lower socio-economic status
- Having experienced postpartum with a previous child
Treating Postpartum Depression
“Most antidepressants are safe in breastfeeding,” says Derish, but she understands why many new parents may want to avoid the drugs while breastfeeding, even if they are experiencing symptoms of postpartum depression. She says there are a number of behavioral interventions she recommends trying first, including:
- Sleeping
- Eating
- Socializing
Each of these can be challenging for a new parent, but it’s important to prioritize them in order to protect your mental health. Derish recommends buying snacks that you can grab and easily eat without preparation such as nuts and grapes. Of course, it may be hard to find time to leave your home and socialize with friends, so Derish suggests having a friend come over from time to time or joining a new parent support group.
How to Talk to Your Doctor About Medicines and Breast Milk
Both Patel and Krutsch agree that the most important thing you can do is to be open with your physician about the medicines, vitamins, and supplements you are using during breastfeeding.
“Despite how much we want to be able to make evidence-based decisions, whenever you don’t have evidence, you still have to make a decision,” Krutsch says. Talking it through with your physician can help you do so. The InfantRisk Center also provides a call center to answer your questions.
Lastly, Krutsch emphasizes that the benefits of breastfeeding often outweigh the minor risks of exposing your baby to medicines.
“Whenever you’re making that risk-benefit evaluation, [remember that] breastfeeding is so beneficial to moms and to babies,” she says.
Remember to Keep Records
Clinical trials rarely include pregnant and breastfeeding mothers. The data scientists do have about the safety of these drugs tends to be from smaller studies or research done in animal models. As MedShadow Foundation founder, Suzanne Robotti recently said in an article about Makena, a drug prescribed to thousands of pregnant women before being removed from the market due to the dangers, “women should obtain physical copies of their medical records, listing all drugs prescribed when trying to get pregnant, while pregnant, and while breastfeeding.”
Breastfeeding has a lot of benefits for mother and baby, but your health is important. You can’t properly care for your baby if your health isn’t being taken care of. In some cases, choosing not to breastfeed so that you can take your medicine and be present for your baby is the best choice!