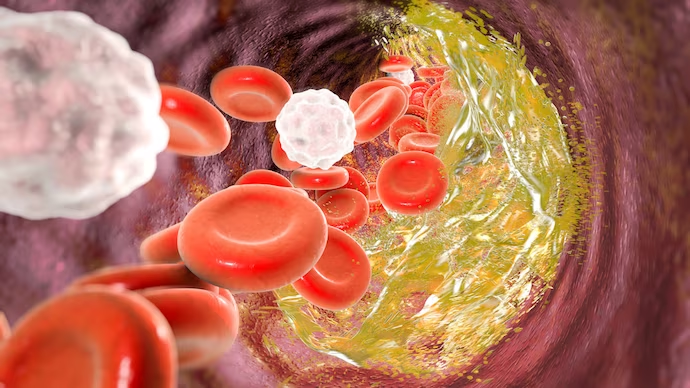
An expensive new cholesterol drug treatment was able to significantly reduce levels of bad cholesterol, though the medication’s ability to lower cardiovascular risk was more modest than expected. The drug, Repatha (evolocumab), is a biologic known as a PCSK9 inhibitor that works by lowering LDL, or bad cholesterol levels. A new study, sponsored by Amgen, Repatha’s manufacturer, found that while those on Repatha saw their LDL levels drop dramatically, their risk of cardiovascular events, such as heart attack or stroke, declined by only 15%. In addition, there was no reduction in the risk of death between those on Repatha and a statin compared to those on a statin alone, researchers reported in the New England Journal of Medicine. Posted March 17, 2017. Via NEJM.
The FDA approved a new Parkinson’s disease medication as an add-on therapy for patients that are experiencing an “off” episode. The drug, Xadago (safinamide), is to be given in addition to levodopa/carbidopa, a standard Parkinson’s treatment. “Off” episodes are when a patient with Parkinson’s is on medication, but it is not working well, leading to symptoms such as tremor and difficulty walking. In clinical trials, the most severe adverse reactions with Xadago were uncontrolled involuntary movement, falls, nausea and insomnia. Posted March 21, 2017. Via FDA.
Prostate cancer treatments have different and varying rates of side effects. A new study examined the incidence of side effects based on multiple types of prostate cancer therapies. Prostatectomy was linked to higher sexual dysfunction and urinary leakage than the other options, the researchers reported in JAMA. At 2 years after treatment, more than 57% of men who had normal sexual function prior to treatment reported poor sexual function after surgery, compared with 27% who reported poor sexual function after external beam radiation, 34% after brachytherapy, and 25% after active surveillance. Researchers say they hope the data helps guide patients and doctors to make better treatment choices. Posted March 21, 2017. Via JAMA.