When Pat (now 71) was in her 40s, her vaginal dryness became so severe that the vaginal tissue would flare with even a gentle wipe. She’d been exposed to a drug called DES (diethylstilbestrol) when she was in utero, which caused myriad health issues as she grew up, and was likely behind the dryness. For her, coconut oil made a huge difference. “If only I had known I was not alone with this personal issue,” she says.
Vaginal dryness is likely more common than you think. It can affect women of any age, but is especially prevalent among those who have already gone through menopause. It’s difficult to estimate how many women are affected, since fewer than half of women who experience it don’t report it to their physicians, but some experts suggest up to 90% of postmenopausal women may experience vaginal dryness. 17% of premenopausal women may experience vaginal dryness, according to the British Menopause Society.
Vaginal Dryness Can Lead to Other Problems
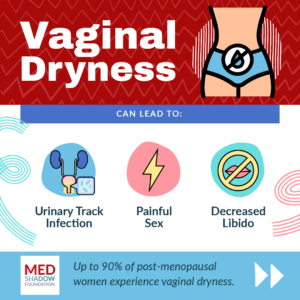
Vaginal dryness can make sexual intercourse painful and lower your libido.
“Vaginal dryness can deeply impact a romantic relationship and healthy sex life. Painful sex is often one of the main symptoms of vaginal dryness, explains Katie Ziskind, a licensed marriage and family therapist and trauma specialist in Connecticut.
When your vagina is dry, the tissue can get inflamed, which causes the burning and pain that many people might assume is a caused by a UTI.
“A lot of women come in and say they have a UTI [urinary tract infection]. They’ll say ‘it burns when I pee.’ They’ll go to their primary care doctor and get an antibiotic but it doesn’t work,” because they don’t have a UTI, says Dorian Jackson, MSN, APN, a Women’s Health Nurse Practitioner at HerAnswer.
There are instances however, in which people with vaginal dryness develop UTIs. The dryness can even raise your risk. Then, you’ll need the antibiotic, but you’ll also need to treat the dryness separately.
Causes of Vaginal Dryness

A Drop in Estrogen
Estrogen naturally drops at two main points in a woman’s lifetime: during perimenopause/menopause and when breastfeeding. After menopause, your estrogen will remain low, but if you’re breastfeeding, your estrogen levels will gradually rise as you begin breastfeeding less frequently. You may also experience a drop in estrogen around the time of your period too, explains Jackson.
Side Effect of Medications
Many medications can cause vaginal dryness. For example, diuretics “which are often prescribed for high blood pressure and fluid retention,” says Nancy Mitchell, Registered Nurse and contributing writer at Assisted Living Center, “work to reduce excess fluid levels throughout the body, but in doing so, they may also reduce blood flow to the reproductive organs, affecting sexual arousal and lubrication.”
They are not the only medications that impact such symptoms.
Decongestant medications prescribed for allergy symptoms can dry out your vagina the same way they dry out your nostrils,” said Mitchell
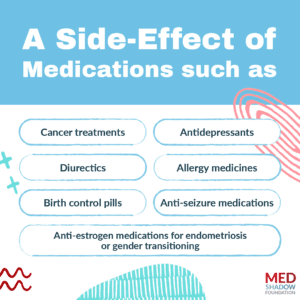
Some other medications that can cause vaginal dryness as a side effect include:
- Cancer treatments
- Antidepressants
- Diuretics
- Allergy medicines
- Birth control pills
- Anti-seizure medications
- Anti-estrogen medications for endometriosis or gender transitioning
Other Causes of Vaginal Dryness
Medications are not the only source of such side effects. Dryness can also be caused by:
- Insufficient foreplay before sex
- Sjorgen’s syndrome, an autoimmune disease
- Ovary removal
- Products such as soaps, perfumes, baby wipes, douches and products that say they’ll make you “smell better” down there.
Treatments for Vaginal Dryness
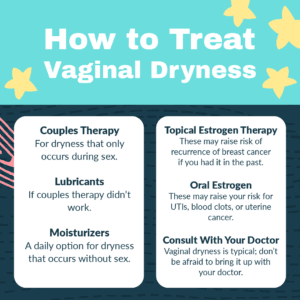
Therapy
If the dryness occurs only during sex, Ziskind recommends talking with your partner and a sex therapist to see if extending foreplay, adding lubricants, or trying new techniques can help. “Couples can gain sex education and sexual confidence from working with a sex therapist,” she says.
Oils
“I like to try the natural stuff first,” says Jackson, explaining that she often advises patients to try applying coconut oil, vitamin E oil, or olive oil to the vagina to see if that helps. Barring an allergy, she says there are rarely any side effects.
“I’ll recommend that women who have dryness use oils daily, not necessarily just related to sex,” she says. If used during sex, however, it is important to note that oils can reduce the efficacy of condoms by breaking the latex.
Coconut oil was a big help to Pat, who started freezing it into very small (she estimates ¼ teaspoon) ice cubes that she’d insert at night. Sometimes the oil would leak out as it melted, so she recommended laying down or using pantyliners.
Kathy, who also has ongoing vaginal dryness, uses a similar technique. She uses a small funnel to pour a mixture of cacao butter and coconut oil into Boba straws, which she then freezes. She inserts a frozen cylinder before bed.
Lubricants and Moisturizers
Lubricants are typically available over the counter and are used during or just before sex to make intimacy more comfortable. They will not help with symptoms unrelated to sex. It’s important to look at the ingredients. They can be water, oil, or silicon-based. Jackson recommends a water-based lubricant, because oil-based lubricants can damage condoms and are more likely to stain sheets and clothing.
Lubricants unfortunately irritated the lining of Pat’s vagina. She says that while the coconut oil was very helpful for daily use, intimacy remained a struggle.
Some lubes include additional ingredients designed to increase sensations like heat or tingling. The lubes may contain menthol or extracts from mint or chile pepper plants that can irritate your vagina. Lubricants can also contain ingredients like parabens that are sometimes found in cosmetics, which can act as endocrine disruptors.
Vaginal moisturizers, on the other hand, are designed to be used daily, or at least several times a week, on a regular basis, much like you’d use moisturizer on your face.
Side effects of vaginal lubricants and moisturizers are unlikely to occur outside of your vagina, but some of the ingredients they may contain can irritate your skin.
In general, avoid any products with added scents.
Topical Estrogen Therapy
Since a drop in estrogen is the most common cause of vaginal dryness, estrogen can help mitigate the problem. However, there is debate about whether vaginal estrogen can raise the risk for a recurrence of breast cancer in certain women who have already survived the disease. For those who haven’t had cancer, the treatment doesn’t increase your risk for a first malignancy. Also, if your symptoms are solely vaginal, you may prefer an estrogen therapy that does not reach your whole body.
There are a variety of ways you can deliver estrogen directly to your vagina using creams or suppositories daily (not before sex). Vaginal rings (soft, flexible rings you can insert in your vagina that releases estrogen continuously for three months), or pessaries, which are devices used to support the vaginal tissues in people experiencing pelvic organ prolapse.
Women experiencing a range of menopausal symptoms including vaginal dryness have other options including using an estrogen-based topical cream on their thighs. This is a good discussion to have with your doctor.
Two studies found that using estrogen creams can increase endometrial thickness which is considered to be a sign that you have a higher risk of cancer. However, authors of a Cochrane Review of studies on vaginal estrogen, that mentions those studies, note that they both used higher than recommended doses.
Jackson says that in some cases, “they may actually notice some bleeding too, because you’re inserting something into these tissues that are already inflamed and dry.”
Oral Estrogen
Ospemifene is a drug that mimics estrogen in your body. Your healthcare provider may prescribe it if you have trouble using vaginal methods, but Jackson says she rarely prescribes oral estrogen for her patients.
“We usually stick with a method that works where it is,” she said. Oral estrogen can cause hot flashes and may raise your risk for UTIs, blood clots or uterine cancer.
Laser Therapy
If the options above haven’t helped your vaginal dryness, your doctor may recommend laser treatment. The MonaLisa Touch and DiVa lasers are devices which your gynecologist will insert into your vagina for 5 minutes. You may feel the device being inserted (which can hurt if you’re experiencing dryness), but you shouldn’t feel the laser itself. Your physician may recommend numbing cream to help with any discomfort. The light is thought to stimulate the growth of healthier vaginal tissue by damaging the existing tissue.
Typically, you’ll receive three or four treatments over the course of 18 months. Then, you may continue about once a year. However, this course of treatment can vary based on your individual symptoms and experience. You may be sore for several days after the procedure. Experts recommend waiting at least five to seven days before resuming sexual activity.
However, these technologies are controversial. Data on their efficacy is limited. The devices are not subject to the same level of FDA oversight as drugs, and an OB/GYN recently wrote for STAT News that she is seeing many patients seeking help for burning, scarring and severe bladder pain as a result of these treatments.
Speak With a Doctor
Most importantly, says Jackson, stigma can stop people from discussing vaginal dryness with their healthcare providers.
“If you’re having vaginal dryness, mention it,” she said. “Don’t be ashamed. It is something that can affect our lifestyle and our enjoyment of life or enjoyment of sex. So speak up about it.”






