Coenzyme Q-10 (CoQ-10) Starts To Diminish As We Age
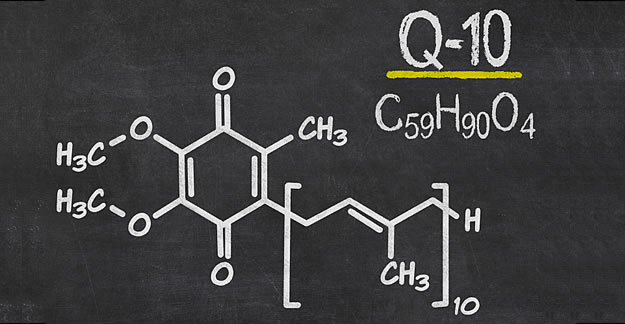
Coenzyme Q-10 (CoQ-10) is a natural antioxidant made by our bodies and found in foods such as fatty fish (salmon and tuna), meats and chicken, peanuts, and canola and soybean oils. Our bodies need Coenzyme Q-10 to protect cells, reduce the risk of developing chronic diseases, and convert food into energy.
But as we age, our levels of CoQ-10 start to diminish. Certain drugs such as statins (used to lower cholesterol) and beta-blockers (for high blood pressure) can also decrease our CoQ-10 levels, as can health conditions such as heart disease, high blood pressure, diabetes, and cancer. (Coenzyme Q-10 levels can be checked by a blood test; but some symptoms include muscle weakness and pain particularly for those taking statins.)
To compensate for these deficiencies—and to offset a host of other problems, including migraines, chronic fatigue, male infertility, and gum disease — millions of people worldwide take CoQ-10 supplements. The U.S. and European market is expected to top $133 million by 2015, according to a report by Global Industry Analysts.
A study of 50 adults of both sexes, aged 40-65, found CoZ-to to be very helpful in lowering muscle pain in about 1/3 of statin users. But seniors who consume Coenzyme Q-10 supplements need to exercise caution: These nutraceuticals can cause problems if combined with other drugs. For example, sinceCoQ-10 has a relaxing effect on blood vessels, it can lower blood pressure levels. If taken with a high blood pressure medication, CoQ-10 can cause blood pressure to drop too low.
Speaking to The New York Times, Roxanne Sukol, MD, a preventive medicine specialist at the Cleveland Clinic’s Wellness Institute, says, “It takes about eight weeks for this effect to kick in, and those who are already on blood pressure medications and choose to take CoQ-10 should do so under the guidance of a doctor.”
CoQ-10 can also reduce the effectiveness of blood thinners such as heparin, warfarin, or even aspirin. While these drugs are used to slow blood clotting, CoQ-10 can have the opposite effect, putting a senior at risk for dangerous blood clots. If a senior is taking a CoQ-10 supplement, it’s important that he or she have their blood checked regularly as the dose of a blood thinner might need to be changed.
Seniors should always tell their physician about their supplement use, particularly if they are taking CoQ-10 in addition to a statin, blood thinner, or beta-blocker.
—Laura Broadwell