Download the full Burnout or Depression Infograph.
Puja Aggarwal, MD, a neurologist, remembers the time six years ago she experienced burnout.
“I was working long hours, socially withdrawn, not sleeping, feeling empty and giving all my time to work. I was not able to show up well as a mother or take care of myself,” Aggarwal explained about the challenging time. After she sought the help of a life coach, she was so inspired by how the guidance helped her achieve a healthier work-life balance that she pursued a life coach certification for herself.
Many of us can probably say we’ve experienced burnout at some point, as the stresses of work, or even home obligations, can overwhelm us and cause us to be exhausted and apathetic and chronically lose sleep. Oftentimes, we feel better when a big project ends or we’re able to take a brief respite from the office. However, with the pandemic and the unrelenting stresses that have come with it well into its third year, you may be thinking that the burnout is never-ending. You may even be wondering if what you initially identified as burnout is actually chronic clinical depression.
You would not be alone. Burnout has surged during the pandemic. Google has reported that searches related to burnout flourished over the past year.
One of the breakout searches in 2021 and 2022 was “burnout versus depression.”
What Is Burnout?
The World Health Organization (WHO) defines burnout as a condition (but not a disease) caused by your occupation. More recently, more and more people are starting to attribute burnout to obligations outside of the workforce, such as parenting and caregiving, from which it can be especially difficult to take time away. That may be making it harder for people to differentiate between burnout, depression or a combination of both, but doing so is crucial to ensuring you get the necessary treatment.
Krista Elkins, a paramedic and registered nurse who has been experiencing burnout throughout the pandemic, notes the main difference between burnout and depression. If you’re experiencing burnout, you feel better whenever you get away from your stressor. “They might find great pleasure in being home, spending time with their family or doing his or her hobbies. Once they return to work, however, the overwhelming feelings of stress return,” she says.
Burnout is especially common among teachers, healthcare professionals and those in other service jobs. Nonetheless, it can happen in any job, including parenting and caretaking. Long hours, lack of support and feeling like you have little control at work can increase your risk for burnout.
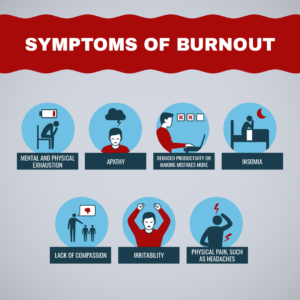
Symptoms of burnout include:
- Mental and physical exhaustion
- Apathy
- Reduced productivity or making mistakes more frequently
- Insomnia
- Lack of compassion
- Irritability
- Physical pain, such as headaches
Burnout Treatment and Side Effects
“The best treatment options for burnout are to alleviate the stressor. In other words, quit their job, or find a different line of work,” says Elkins. She herself is transitioning out of the medical field toward writing after experiencing burnout.
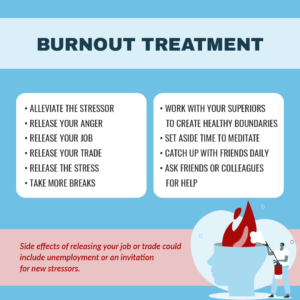
Taking her advice is easier said than done. If you can’t or don’t want to leave your job, you can also try to find ways to take more breaks, work with your superiors to create boundaries and improve your working conditions or ask friends and colleagues for help. The CDC suggests making small changes, like setting aside time to meditate or catch up with friends each day.
MedShadow has more suggestions, including guided breathing exercises, in our article: Stress Need Not Be Your Constant Companion.
What Is Depression?
Like burnout, depression is characterized by fatigue, lack of interest in activities you once enjoyed and a host of physical symptoms. The main difference, experts say, is that the symptoms persist even if you’re taking a break from your stressors. To be diagnosed with depression, you need to consult with a physician.
Over the course of two weeks or more, if you feel any of these symptoms nearly every day, you may be suffering from depression, according to the National Institute of Mental Health.
- Persistent sad, anxious or “empty” mood
- Feelings of hopelessness, or pessimism
- Irritability
- Feelings of guilt, worthlessness or helplessness
- Loss of interest or pleasure in hobbies and activities
- Decreased energy or fatigue
- Moving or talking more slowly
- Restlessness or having trouble sitting still
- Difficulty concentrating, remembering or making decisions
- Difficulty sleeping, early-morning awakenings or oversleeping
- Appetite and weight changes or both
- Thoughts of death or suicide or suicidal attempts
- Aches or pains, headaches, cramps or digestive problems without a clear physical cause that fail to ease, even with treatment
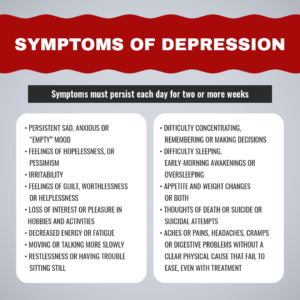
Symptoms of depression
It is normal to grieve, feel sad or even depressed in response to certain difficult events. If those feelings become overwhelming, speaking to a therapist or seeking other treatment may help.
Depression Treatment and Side Effects
There are many ways to treat depression, and they’re often most effective in combination.
One of your first steps might be to speak with a therapist. A therapist may be able to help you process emotions and develop strategies for handling stress.
A therapist might also encourage you to develop some healthy habits. For example, regular exercise and healthy sleep habits are known to mitigate symptoms of depression.
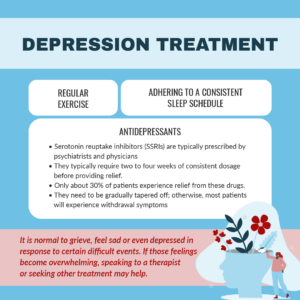
A physician or psychiatrist might prescribe drugs like the class of antidepressants called selective serotonin reuptake inhibitors (SSRIs) as well. It’s important to know that you may need to take these drugs for two to four weeks before you start feeling relief from your symptoms. Know also that they don’t work for everyone. Only about 30% of patients report improvements from most antidepressants, and many others report harmful side effects. You may need to try different drugs to find one that helps you. If, eventually, you no longer need antidepressants, work with your doctor to gradually taper your dose. Otherwise, you may experience withdrawal symptoms.
Side effects of antidepressants are common. Many of these drugs carry warnings regarding suicidal ideation and behavior. It’s vital to spend time talking with your doctor about what you might expect and what to do if you experience any of the following:
- Suicidal thoughts or attempts
- New or worsening depression or anxiety
- Increased agitation, irritability or restlessness, which can be symptoms of akathisia
- Panic attacks
- Insomnia, or other sleep problems
- Acting aggressive, impulsive and violent or both
- Posing a threat to yourself or other people
- A significant increase in activity and talking, symptoms of mania
- Other unusual behavior or mood changes






