As you age, things change. You likely notice the little things over time, such as feeling like you pulled a muscle just by sneezing, or maybe you wake up with aches and pains that seemed to develop in your sleep.
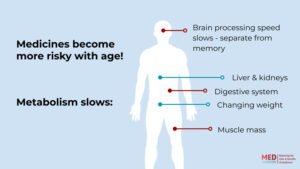
But, there is more to the story. Your body is going through a lot of change. And, by 65, the medical industry has determined that enough change has occurred that it is worth noting unique “rules of thumb” to follow for the age group. In general, your body is slowing down. Some drugs stick around longer in fatty tissues, others take longer to filter through your liver and kidneys.
In most cases, this means that you’ll need to lower your doses to avoid more intense side effects as each dose you take lasts longer. But sometimes, a delay in processing makes the drugs less effective, and you’ll need a higher dose.
“Just because you’ve been taking the same dosage forever does not mean that’s going to be the right dose as you age,” says Sun Jones, DNP, a faculty member at the University of Phoenix College of Nursing.
Let’s explore some of those changes, what they mean for your personal health, and medication changes for seniors you should know about.
Changes to Your 65-Year-Old Body
Remember puberty? Sometime around your preteen and teen years, your body went through those awkward stages of change? From hair in new places, to strange feelings and hormones, you were going through a lot.
Turning 65 is similar. There are changes going on during this approximate age (a bit before and a bit after for some; we are all different!) too.
These changes can include aching of age-deteriorated joints, particularly if excess weight is an issue. A weakening of your bones and muscles (explaining some of those aches and pains), struggles with brain processing (why am I in this room again?), structural changes to your large intestine (please pass the prunes), decreases in bladder elasticity (the need to pee more often), and less skin elasticity, too (not another wrinkle there).
“As people age, our bodies start to process medications differently, which increases the risk of adverse side effects,” explains Laura Herman, CNA, an elderly Care Specialist with Safer Senior Care. Herman is a former Certified Medication Aide, and former Residential Care and Assisted Living Administrator with 25 years of experience supporting seniors and their families including in Skilled Nursing, Residential Care, Memory Care, and In-Home Care environments. “For example, the liver and kidneys, which metabolize and eliminate drugs, work more slowly in older adults. This can result in medication remaining in the body for longer periods – heightening the likelihood of side effects, even when taking doses as prescribed.”
Some of your body changes impact the efficacy of medications, too. Overall, things take a bit more time. You likely have slowed your pace on the staircase, for example. So too are the processes inside your body slowing, including the metabolism of medications.
The way your body uses medication changes when you’re 65. These changes make understanding their side effects even more important.
Muscle Can Become Fat
As your muscles weaken, it’s true. You can become a bit shakier, requiring handles on nearly anything, assistance on or avoidance of stairs, and an overall less stable frame. While these signs of aging are frustrating, they also mean you are at greater risk for medications that have side effects such as dizziness, vertigo, light-headedness, and unsteadiness.
Think of your balance, say, in your 20s. For one thing, it was probably far better than it is in your 60s and beyond. But secondly, you also probably would not have had life-altering harm if you fell.
As you age, more of your muscle tissue turns to fatty tissue, explains Jones. And the effects are two-fold. First, many drugs are fat-soluble, meaning they can be stored in your fatty tissue. More fatty tissue means more space for some drugs to stick around in that fatty tissue, raising the risk of side effects. That’s one reason you may need to lower your dose.
Secondly, having strong muscles is important for maintaining balance. Losing them increases your risk of falling down. Each year, one out of four persons 65 and over fall.
Falls when you’re over 65 can be truly life threatening. Likely outcomes, such as broken bones and brain injury, can be very serious on their own. Hip fractures, for example, which averages a result of 300,000 seniors hospitalized for falls annually, have been shown to closely correlate with mortality. A 31-year study in published in 2019 found that the one-year mortality rate of seniors with a hip fracture is 21%, if that fracture is surgically repaired.
Even with treatment, such massive injuries at an advanced age can be debilitating, destroying the quality of life, the ability to remain mobile, and live without pain.
Many drugs can cause dizziness and lightheadedness as a side effect, that combined with weaker muscles hindering your balance can spell disaster. You may need to change your dose when you’re a senior to avoid falls. Additionally, make sure you speak with your healthcare provider about any signs of dizziness, and find exercises that you enjoy enough to do regularly to help maintain your strength and balance.
Your Aging Liver
Your liver is the body’s filter, and nearly all medications, prescription or over-the-counter (OTC), not to mention herbal supplements, vitamins, and clinical treatments, are processed there. All of the blood in your body is filtered by the liver. It removes “poisons” such as prescribed drugs or even alcohol from the blood, which means it is working over-time when you use more medications and supplements..
As you age, your liver is changing. Your liver is changing at the cellular level, and those changes mean it takes longer to process your medications, leaving them circulating in your body longer. It is processing more slowly. In most cases, this means your medications stay in the body longer.
You can think of the filtering process as a line of traffic. The liver is much like a traffic light, slowing incoming traffic, requiring a longer and longer “red light” with age. As traffic backs up, each “car” (or medication) has to wait longer in line for their turn at a “green light” (healthfully processed blood). That means more and more cars are in your body. A dose that was appropriate for you before may be too high in this new traffic jam.
Still, some drugs need to be broken down in the liver in order to be effective. If the liver is struggling to process these types of drugs, they may no longer be as useful to you as they once were.
As Your Kidneys Age
Much like the liver, nearly all medications will pass through the kidneys, too. In fact, medications are the cause of 20% of all acute renal failures in the United States. Kidneys remove waste from the blood and convert it into urine.
Scientifically speaking, your kidneys experience reduced filtration rates. Your blood flow to the kidneys is also reduced with age. Because of these two known factors, your kidneys are processing at a slower speed, overall. This means your body will more slowly process waste out of your blood, and produce the urine, meaning drugs may stay in your system longer than they used to at younger ages. Just like the liver’s “traffic,” so too is the waiting line for the kidneys lengthening the older you get.
Underrepresentation of Seniors in Trials
For a new drug to be approved by the Food and Drug Administration (FDA) for market, its clinical trials have shown some efficacy. It may be a drug more effective than what the current market has to offer. It may be an alternative to available treatments, with better results or fewer risks. Overall, the studies must show that its health benefits outweigh its risks.
However, what happens when the drug was tested on a far younger audience than its senior users? Studies have shown that in trials involving diseases that affect people of all ages,, only 9% of trial participants were aged 65 and older, and only 1% were 75 and older. Even when the disease was commonly associated with seniors, only 57% of the included patients were aged 65 and older and 22% were aged 75 and older.
In short, this means that these medications, though approved for use in seniors, are not well tested on this population. This leads to more side effects being discovered as they’re used in the “real world.”
Studies have made it clear that FDA-approved medications often turn up with more serious and side effects become a more realistic possibility the longer the drug has been used in actual patients, or in those “real world” uses. In other words, clinical trials cannot accurately capture all potential side effects due to their limitations. Instead, serious adverse reactions become known far after the drug’s initial approval. Some side effects are rare and only show up after the drug has been tested on far more people. The trials may not include enough elderly people in initial testing, or other those taking commonly used medications, like a statin, at the same time as the new drug.
“The safety of new agents cannot be known with certainty until a drug has been on the market for many years,” concludes one 2002 study, which reviewed drugs from 1975 to 1999. The same study notes that 20% of medications approved during that time period later required black box warnings or were withdrawn completely from the market. (A black box warning means that when a drug causes “serious adverse reactions or special problems occur, particularly those that may lead to death or serious injury.”)
Impacts Vary in a Geriatric Body
Trials often enroll mostly middle-aged persons. The effects of drugs on those 65+ may be different from those seen in middle-aged participants. Researchers frequently leave seniors out of clinical trials, as noted above. This means we don’t always know how they will be impacted. It is clear that the true side effects of medications may only be revealed in the elderly community as they are dispersed into real-world situations.
“This situation [healthy, middle-aged adults] is seldom the case in a clinical setting where physicians have patients who present with chronic kidney disease or other ailments, and who may take numerous medications with potential drug interactions,” explains one 2023 report. ”Also, patient age is a significant factor in determining the accurate half-life of a drug, particularly for pediatric and geriatric patients in which drug metabolism and thus half-life can vary significantly from a healthy middle-aged adult.”
Specialists called pharmacokineticists, spend their entire careers studying the variations in how we absorb and metabolize drugs. There are a million reasons why you may respond differently to a drug than people in the clinical trials did. Along with your age, some factors that can change the way you metabolize drugs are:
- Absorption
- Distribution
- Metabolism
- Excretion
With PK, general recommendations for age groups can be created, though still provide only an umbrella statement. Individuals’ unique body compositions, age, gender, race, and physiological factors, not to mention additional drugs, foods, or supplements that may interact, are still factors that must be considered on a patient-by-patient basis.
Herman agrees that, while an aging body’s changes are partially responsible for the slower processing of medications, such rates can also vary person to person.
“Additionally, changes in body composition (muscle mass or fat distribution) can impact how drugs are processed within the body,” she says.
Multiple Meds
Nine out of ten seniors are taking a prescription drug. In fact, most people aged 65 to 69 take an average of five prescriptions a year. Numbers don’t massively change with genera (with approximately 44% of men and 57% of women older than 65 years taking five or more medications per week).
Even more alarmingly, in the United States, 12% of both men and women are taking 10 or more medications per week!
That makes for a long list of potential side effects! And it’s a lot of stress on your liver and kidneys, which are forced to process and filter medications, no matter how they enter the body.
“Because managing multiple health conditions may require several specialists prescribing medications for different conditions, older adults are at high risk for dangerous effects of
Polypharmacy – taking multiple medications concurrently,” says Herman. “This increases
the likelihood that some of the drugs will interact poorly with each other, causing side effects like loss of appetite, confusion, or dizziness which can significantly impact an older person’s safety and quality of life.”
Combining many pharmaceuticals at once is often referred to as “polypharmacy” in the medical field. The complications can be compounded as drugs often interact with one another, increasing or decreasing both efficacy and side effects. It can be hard to tease apart the effects of one drug from another drug or even symptoms of a condition. You may think you’ve developed new problems such as mild cognitive decline, when in fact, it’s just a side effect of medication you’re taking. or adding to adverse reactions due to mixing.
Jones says it’s crucial to talk to your doctor about any new symptoms you feel and ask if they could be new side effects caused by drug interactions.
Take the story of Erin, for example, an elderly woman taking 24 medications, who didn’t even have the energy or desire to speak to her family physician when they first met. After her physician took her off some meds and lowered the doses of others, Erin felt hope again, and told her doctor she couldn’t wait to see her great grandkids. Read more about Erin, and find other deprescribing success stories in MedShadow’s Cutting Down on Medications for Time with the Great Grandkids.
Drugs to Steer Clear of as a Senior
With all of these changing factors, how is a senior to know what is and is not safe to take? Ideally, you will speak individually to your healthcare providers to determine what is best for your unique circumstances whether you need to change your medications when you’re 65 or older. To assist both you and these professionals, however, there is a regularly-updated guide to help make recommendations to the senior audience.
The Beers Criteria
Don’t get excited and crack open that six pack. This is the name of American Geriatic Society’s (AGS) guidelines. The guide, dubbed the Potentially Inappropriate Medications (PIM) in Older Adults is actually named for its developer, Mark H. Beers, MD, who created the list in 1991 as a student at the University of California, Los Angeles. The AGS reviews and updates the list every three years.
The recommendations for seniors is one of five sections, the others including lists for those with certain health conditions, risky drug interactions, harmful side effects that outweigh benefits, and a section of drugs to avoid for those with renal impairment.
The list itself, which you can read here with its most recent 2023 updates, contains hundreds of specific medications across 30 pages of content. However, understanding the categories can help seniors to keep an eye out for themselves and talk to their doctors about medication changes when you’re 65. The following is a list of categories of medication that seniors should be cautious about taking, or minimally understand the risks that come with them:
- Antihistamines
- Cardiovascular/Antithrombotics
- Antidepressants
- Antiparkinson’s medications
- Antipsychotics
- Barbiturates
- Benzodiazepines
- Endocrine/hormonal drugs
- Insulin
- Sonfonylurias
- Desiccated thyroid
- Proton Pump Inhibitors (PPIs)
- GI Antispasmodics
- NSAIDs
- Muscle relaxants
How Those 65+ Can Protect Themselves
The Beers Criteria creates lists that contain potentially inappropriate medicines for those 65 and over. Your personal health condition could make a medicine on the Beers Criteria exactly the right med for you. You will need to work with your doctor to be sure they are firstly aware of all medications you are taking and any drug or dose changes when you’re 65 that you’ll need.
Advocate for Yourself
The first step to protecting yourself is by advocating for yourself and speaking up! You are in charge of your body, what you put into it and what you do not. Education goes hand-in-hand with advocating for yourself. To do so, seek out trusted, uninfluenced resources to be sure you understand the risks and benefits of medications. Once you make an educated decision for your own body, don’t be afraid to stand your ground, ask your questions, and be sure your healthcare professionals know your preferences.
Don’t Assume Cognitive Decline or Depression is Normal
Yes, many of us do start to think a little more slowly and get a little more forgetful as we age, but it’s not alway inevitable. In many cases, it’s actually due to side effects of medications you’re taking! If you notice confusion or forgetfulness in yourself or your loved one, be sure to ask your healthcare provider if it could be your prescriptions, says Jones.
She also recommends continuing to challenge your brain regularly.
“We found in studies that, if they keep up with the cognitive functioning, doing things such as reading books and keeping up with their professional scene [even if they’re retired], they have less chance of developing dementia.”
She added that monitoring mental health and loneliness is also important as people age and may become more isolated.
“Mental health is a biggie,” says Jones. “It has a direct relationship with physical health.”
For more dementia-preventing strategies, check out MedShadow’s Prevent Alzheimer’s: Lifestyle Modifications You Can Make Today.
Create a List of All Medications
Create a list of all medications that you take. This includes prescription drugs, OTC medications, and even vitamins or supplements you take by choice.
“It’s crucial to maintain a single master medication list of all prescription and over-the-counter medications,” says Herman. She said the list should also include “supplements, alcohol, marijuana products, or other drugs for a single doctor or geriatric pharmacist to review regularly.”
Creating a medication list and having it examined by a doctor or pharmacist who specializes in geriatric medicine is one of the first steps she recommends to older patients and their caregivers.
Seek the Care of a Geriatric Specialist
Yes, the word may make you cringe, but by 65, it is official. You are a “senior” and require specialized care. Parents take children to a pediatricians because they specialize in the care of young children.
So many patients, she says, remain with the same family doctor for years, and don’t think to make a change by their mid-60s.
Herman says seeking a geriatric care specialist is one way to ensure that your doctor is well-versed in seniors’ unique needs.
“Doctors who specialize in geriatric medicine are familiar with proper dosing guidelines for older adults, but many general practitioners don’t seem to take these into account,” says Herman. “Older adults often take the same dose of the same medication year after year, without much thought as to whether it’s still necessary, or if the dose may need to be adjusted.”
One patient, Julie, who just turned 65, says she learned about the need for medicinal changes from her physician who recommended a lower dose of her selective serotonin reuptake inhibitor (SSRI).
“I never knew that dosages changed when you hit 65,” she says. “I was surprised my doctor recommended the lower dose.”
Julie says that the drug citalopram (Celexa) is not recommended to be taken by adults older than 60 years in doses over 20 mg per day. She says she later learned the FDA warned of a very serious side effect should she not lower her dose.
“There is a potential risk for QT prolongation,” Julie says her doctor informed her about at her last visit.
QT prolongation means that the heart muscle takes a longer time to contract and relax than usual. It can alter heart rhythms and lead to cardiac arrest, not side effects Julie wanted to risk.
Julie opted to reduce her prescription to avoid potential side effects, per her doctor’s recommendation, and was glad to have a healthcare professional watching out for her. She says others her age should check their medications with their doctor to be sure the dosages and drugs you change when you’re 65 are being monitored.
Coordinate Your Care
Another challenge faced by older adults is that, also by now, we tend to need the aid of multiple specialists. You may see your GI doctor for your gastrointestinal reflux disease (GERD), but go to your sleep specialist for your apnea, and an OB/GYN for your annual feminine exams. These specialists may not be in the same network or corporate chain. This may mean their files are not always properly shared and accessible by all healthcare providers.
Additionally, while technology has provided amazing advances in the medical field, it isn’t a perfect system. You may hope your medical records travel with you from doctor to doctor, but it isn’t always the case. Asking for print copies you can physically carry along with you may prevent polypharmacy complications with medication interactions.
Patients should minimally be sure that each doctor, no matter what they treat, is aware of all medications and treatments you take. You may not think your neurologist needs to know about your recent dental operation, but if it required any medication like sedation, it can be incredibly relevant to future prescriptions she may need to write.






