Do you ever have acid reflux and wonder if it’s really a heart attack? Do you see headlines every winter warning of the dangers of “Holiday Heart Syndrome” and find yourself wondering if the stress and indulgence of the holidays can actually cause a specific heart disease? MedShadow explains everything you need to know about the conditions, their treatments, and the side effects of drugs used to treat heart disease.
How the Heart Organ Works
What Is Heart Disease?
Heart disease is any condition that affects the way your heart functions. Heart disease can be structural, for example, a birth defect that leaves an extra hole between two sections of the heart could cause a heart a murmur. Heart disease can also be caused by infections or scar tissue that weaken the heart muscle or blockages in the arteries that prevent blood flow.
Types of Heart Disease
Heart Attack (Myocardial Infarction)
Plaque within the arteries of your heart can break off. When that happens, it forms a blood clot that can block blood flow to your heart. The longer the parts of your heart go without the oxygen and other nutrients that blood typically delivers, the worse the damage to your heart. Heart attacks can be
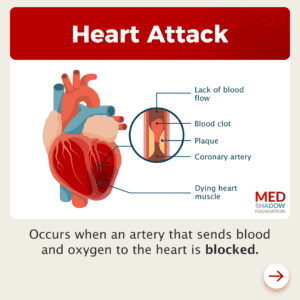
fatal, but if doctors are able to restore blood flow to your heart before too much damage occurs, you can survive and heal.
Symptoms of a heart attack
The most common sign of a heart attack is tightness, pressure, or pain in the chest but not everyone feels this symptom, and there are some other signs. Women are more likely than men to experience the following symptoms of a heart attack:
- Discomfort in either arm (not just the left arm)
- Discomfort in the jaw, neck, back, or stomach
- Shortness of breath
- Nausea or vomiting
- Lightheadedness
If you suspect you might be having a heart attack, do not wait. Go to the emergency room immediately. If you are correct, the faster a doctor can treat it, the less damage will be done to your heart.
After a heart attack, many patients are prescribed drugs to help prevent another one, such as
- Blood thinners
- Aspirin
- Statins
- Beta blockers
- Calcium channel blockers
In October 2023, researchers also found that after a heart attack, patients who received a Chinese herbal medicine, Tongxinluo, alongside standard treatments, were less likely to have another heart attack or several other complications than those who only used standard treatments over the next year. The most commonly reported side effect of the treatment was nausea.
Several lifestyle changes can also help lower your risk of experiencing another heart attack, such as:
- Cardiac rehab
- Diet
- Exercise
- Relaxation
Heart Failure
Heart failure occurs when your heart isn’t pumping effectively enough to get blood, oxygen, and nutrients to all your tissues. At first, the heart starts to make up for its inability to pump by growing larger or pumping faster. Your blood vessels may narrow and your body may start prioritizing blood flow to certain organs at the expense of others. Many people don’t experience symptoms at first, but eventually you may feel:
- Fatigue
- Shortness of breath
- Swelling of the feet, ankles, or legs
- Rapid heart rate
- Confusion
- Lack of appetite
- Coughing
Heart failure can be a result of strain on the heart due to a variety of underlying conditions such as high blood pressure, birth defects that affect the structure of the heart,or myocarditis, but it can also be a side effect of certain medications, such as chemotherapy and radiation.
If you’re diagnosed with heart failure, your healthcare provider may prescribe:
- ACE Inhibitors
- Angiotensin II Receptor Inhibitors
- Beta Blockers
- Diuretics
- Hydralazine and isosorbide dinitrate
- Aldosterone Antagonists
Heart Rhythm Disorders (arrhythmias)
An arrhythmia is any abnormal heart rhythm. It can mean your heart is beating too fast or too slow, or you might feel like it’s skipping a beat, for example. These conditions can have many different causes such as stress, scarring of the heart tissue, changes in blood flow, and even side effects of heart medications.
Atrial fibrillation is one of the most common heart rhythm disorders, and both its symptoms and risks can differ between women and men. Women are more likely to have longer-lasting episodes of atrial fibrillation and experience fatigue as a symptom than men. They’re also at higher risk of stroke as a complication of the condition.
Some arrhythmias quickly resolve on their own with no symptoms, but others may last longer, causing:
- shortness of breath
- dizziness
- chest pain
- sweating
- fatigue
- rarely, cardiac arrest.
If you have an arrhythmia, your healthcare provider may prescribe:
- blood thinners to reduce your risk of having a stroke
- beta blockers to reduce your heart rate
- calcium channel blockers which lower blood pressure
- antiarrhythmic drugs which can interrupt abnormal heart rhythms but are known to come with many side effects
Cardiomyopathy
Cardiomyopathy is a condition that weakens the heart and makes it more difficult to pump blood and maintain a healthy rhythm. In most cases, your heart grows larger, and the tissue gets thicker and stiffer. There are many types of cardiomyopathy. Some are caused by genetics, while others develop due to other conditions. Its cause isn’t always clear.
Symptoms of cardiomyopathy are similar to those of other heart diseases and can include:
- Shortness of breath
- Swollen legs, feet or ankles
- Dizziness
- Fainting
- Chest pain
- Arrhythmias or murmurs
Your healthcare provider may prescribe:
- ACE inhibitors to lower your blood pressure
- Beta blockers to slow your heart rate
- Calcium channel blockers to slow your heart rate
- Digoxin to slow your heart rate
- Antiarrhythmics to prevent abnormal heart beats
- Diuretics to remove water and sodium form your body
- Anticoagulants to prevent blood clots
- Anti-inflammatories
Myocarditis & Pericarditis
Myocarditis and pericarditis are inflammation to different parts of your heart. Most often, the inflammation is caused by an infection, such as COVID-19, but it can also be a side effect of medication or an autoimmune disorder. Pericarditis can also be caused by heart attacks, strokes, injuries or surgeries.
You may experience:
- Fever
- Flu-like symptoms
In addition to symptoms that are common to many forms of heart disease such as:
- Chest pain
- Lightheadedness
- Fatigue
- Shortness of breath
- Irregular heartbeats
Inflammation in the heart often clears up on its own, but your healthcare provider may prescribe:
- Antibiotics, antivirals, or antifungals to treat an infection
- Anti-inflammatories that can temporarily reduce inflammation around your heart
In some cases, your physician may recommend surgical procedures.
Infective Endocarditis
Endocarditis is a dangerous bacterial infection that makes its way through the bloodstream into the lining of your heart. It’s rare but maintaining your oral health and avoiding intravenous drugs can help reduce your risk. If you contract endocarditis, your physician may prescribe antibiotics.
What Are the Symptoms of Heart Disease in Women?
You may have heard by now that the symptoms of a heart attack are different for women than they are for men. That’s true for a variety of types of heart disease. Women with heart disease tend to experience more of the atypical symptoms on the list. For example, what feels like a combination of acid reflux and fatigue may really be a heart attack. Men are more likely to feel the tight chest pressure that’s become synonymous with the condition.
For Cherée Johnson, it felt like a year of sharp, but brief chest pains that woke her up at night but quickly faded. One day, the chest pain happened while she was gardening, then returned while she ran errands and at dinner, she started having trouble swallowing. By that night, she collapsed. Her husband rushed her to the hospital where the doctor discovered she had been having a heart attack for 18 hours. It turned out she had a rare heart disease that blocked her artery while she was at rest, eventually leading to a heart attack. Now with medication, her risk of experiencing another heart attack is low.
When it comes to atrial fibrillations, some of the most common abnormal heart rhythms in older adults, the symptoms in men are more likely to be short-lived while women may experience fatigue, shortness of breath and racing heart for a longer period of time. Women with the heart disease atrial fibrillation are also at higher risk than men are to experience a stroke.
Conditions That Put You at Risk of Heart Attacks or Strokes
There are different conditions that a person may have that contribute to their likelihood for heart attacks or strokes.
Coronary and Peripheral Artery Diseases (CAD and PAD)
In both diseases, your arteries, which carry blood away from your heart, narrow because fatty plaque has built up inside them. Both put you at higher risk for heart attacks.
CAD, which affects the arteries closest to the heart, can cause:
- Chest pain
PAD, which affects arteries farther from the heart, can cause:
- Leg pain
- Cold in a particular limb
- Erectile dysfunction
- Less nail and hair growth than usual
If you are diagnosed with CAD or PAD, your physician may recommend drugs to reduce your cholesterol or blood pressure or reduce your risk of arrhythmias with treatments such as:
- Beta blockers
- Calcium channel inhibitors
High Blood Pressure
High blood pressure is often called the “silent killer” because it has very few symptoms, but uncontrolled high blood pressure raises your risk for heart attacks, strokes and other heart diseases. You’re most likely to be diagnosed at a routine visit to your healthcare provider.
If you’re diagnosed with high blood pressure, your healthcare provider may recommend increasing your physical activity, limiting salt intake or taking one or more of the following:
- ACE inhibitors
- Beta Blockers
- Diuretics
- ACE II receptor blockers
- Calcium channel blockers
- Vasodilators
- Alpha blockers
- Alpha-2 receptor agonists
- Central agonists
- Peripheral adrenergic inhibitors
High Cholesterol
LDL cholesterol (the bad kind) can clog your arteries and increase your risk for conditions like CAD and PAD. You likely won’t have symptoms of high cholesterol and will be diagnosed by a blood test at a regular appointment with your healthcare provider.
In addition to increasing your physician activity and lowering the amount of cholesterol you eat, your healthcare provider may prescribe Statins.
Statins are the most common drug prescribed for high cholesterol, though you may also be prescribed:
- Cholesterol absorption inhibitors
- Bile acid sequestrants
- PCSK9 inhibitors
- Adenosine triphosphate-citrate lyase (ACL) inhibitors
Can Alcohol or Energy Drinks Cause Heart Disease?
For a long time, researchers claimed that alcohol, in moderation, could reduce your risk of heart disease, but new studies (and re-analysis that investigated conflicts of interest in many of the old ones) have shown that any amount of alcohol can hurt your heart. Of course, while light drinking does raise your risk of heart disease, heavy drinking increases your risk much more. Over time, alcohol can raise your risk of heart disease, but drinking alcohol can also raise your immediate risk of heart diseases like atrial fibrillation in the hours after you drink. It’s one of the reasons that the holiday season is particularly rife with cases of atrial fibrillation.
Like alcohol, energy drinks with high quantities of caffeine may trigger episodes of atrial fibrillation or other heart diseases caused by irregular heart beats shortly after you drink them.
Is My Risk of Heart Disease Hereditary?
Roughly one third to half of your risk of the most common heart disease, coronary artery disease, comes from your genes, according to a large Veterans Affairs study published in 2022. However, many of the risk factors for heart disease are not hereditary such as your diet, level of physical activity and age.
Lowering Your Risk for Heart Disease
There are some risk factors for heart disease that you may not be able to control such as genetics, birth defects, and pollution exposure, but there are many more risk factors that you can control. These lifestyle changes can be helpful, even if you’ve already been diagnosed with heart disease.
Physical Activity
One of the best ways to lower your risk of heart disease is to get more physical activity. Women and men who reported participating in any amount of physical activity had a 36% and 14% lower risk of dying from cardiovascular disease than those who didn’t report any, according to February 2024 study of more than 400,000 people. Additionally, while only one out of every five women reported doing exercises that strengthen muscles such as lifting weights and doing squats or pushups on a weekly basis, doing so reduced their risk of dying from heart disease by 30%. Men who did two or three muscle strengthening activities per week had an 11% lower risk of dying from heart disease than their counterparts who did not. Essentially the takeaway of the research is that getting more exercise is better than less, and it’s ideal to get a combination of cardiovascular exercise such as walking, running, biking or swimming and muscle strengthening exercises such as weightlifting or bodyweight exercises.
Here are some exercise resources from MedShadow to help you get started:
The Guide to Strength Training for Beginners
Outdoor Workouts, When You Don’t Feel Like Running
Playlists and Podcasts to Power Your Next Walk or Workout
Diet
Eating a diet that’s low in sodium, saturated fats and cholesterol can go a long way toward protecting your heart. The Mediterranean diet, which emphasizes fruits, vegetables, healthy fats, legumes, whole grains, fish, and lean meats can be a great place to start.
Here are some diet resources from MedShadow:
Eating out on a low sodium diet
Relaxation
Stress can raise your blood pressure. Make sure you’re making time regularly to decompress.
Here are some relaxation resources from MedShadow:
Stress Need Not Be Your Constant Companion
How to Relax During the Holidays
8 Best Breathing Exercises on Instagram
Instagram’s Best Booze-Free Ways to End the Day
Other ways to lower your risk of heart disease:
- Do not smoke
- Limit alcohol intake
- Get your flu shot and wash your hands to minimize risk of infections that can strain your heart
Side Effects of Common Medications for Heart Disease
ACE Inhibitors and Angiotensin Receptor Blockers help lower your blood pressure and prevent additional tissue damage after you’ve had a heart attack.
These medications include:
- Prinivil (lisinopril)
- Accupril (quinapril)
- Fosinopril, captopril, Vasotec (enalapril)
- Perindopril, Altace (ramipril), trandolapril
A dry cough is a common side effect. Some people may experience dizziness or fainting if their blood pressure drops lower than it should. They can also cause high potassium or stress the kidneys.
When Harley Sears, a hypnotist based in Kansas City, Missouri, was prescribed lisinopril, an ACE inhibitor, he developed a cough severe enough to interfere with his work. He started meditating, and five months later, he says, his physician took him off the medication.
Beta Blockers lower your heart rate and blood pressure.
Examples of beta blockers include:
- Toprol-XL (metoprolol)
- Coreg (carvedilol)
- Brevibloc (esmolol), bisoprolol
Healthcare providers will often prescribe them after you’ve had a heart attack, especially if it caused heart failure.
Cold hands and feet, fatigue, dizziness, weight gain, and nausea are common side effects. Less commonly but more seriously, beta blockers can slow your heart rate too much or cause shortness of breath.
Diuretics flush water and sodium out of your body, helping reduce the workload on your heart and improve symptoms of heart failure and high blood pressure.
Some diuretics are:
- Lasix (furosemide)
- Bumex (bumetanide)
- Demadex (torsemide)
- Diuril (chlorothiazide)
- Midamor (amiloride)
- Chlorthalidone, hydrochlorothiazide, indapamide, Zaroxolyn (metolazone)
- Dyrenium (triamterene)
More frequent urination is a common side effect. It’s important to make sure you’re hydrated, especially when it’s hot outside. John Michael Sefel, a writer and researcher, went to the hospital more than once after experiencing headaches, dizziness and nausea due to the heat. He only recently learned that the diuretics he’s been prescribed may be putting him at risk.
Your blood pressure could lower too much, leading to dizziness and fainting. The most serious possible side effects are reduced kidney function and altered levels of important minerals such as potassium, magnesium, and calcium. Uric acid can also build up in your blood, causing gout.
Calcium Channel Blockers limit the electrical activity in your heart, allowing your blood vessels to widen and slow your heart rate. They typically treat abnormal heart rhythms and chest pain.
Calcium channel blockers include:
- Norvasc (amlodipine)
- Cardizem (diltiazem)
- Nicardipine, Procardia (nifedipine)
- Nisoldipine, Calan SR (verapamil)
The most common side effects include gastrointestinal distress, dizziness, flushing, headaches, fatigue, and swelling in the feet and legs. Less common, but more serious, the drugs can cause jaundice, rapid heart rate, and worsening chest pain.
Anticoagulants, Antiplatelets and Aspirin are blood thinners prescribed to prevent the formation of blood clots, especially in people with atrial fibrillation, a type of irregular heart rate and heart failure.
Some common anticoagulants are:
- Coumadin (warfarin)
- Pradaxa (dabigatran)
- Xarelto (rivaroxaban)
- Eliquis (apixaban)
- Savaysa (edoxaban)
Antiplatelets include:
- Plavix (clopidogrel)
- Brilinta (ticagrelor)
- Aspirin
These drugs can interact with foods that contain vitamin K, so your healthcare provider may recommend that you monitor your intake of green, leafy vegetables. They also interact with many other drugs, you be sure to review a complete list of anything you take, including over-the-counter drugs and supplements to review with your provider.
You may also experience dangerous bleeding or shortness of breath.
Low-dose aspirin was once commonly prescribed to prevent heart attacks and strokes in people at risk, but scientists no longer think it’s effective for everyone. Experts debate whether it helps for people who have already had a heart attack or stroke.
Statins lower your cholesterol to reduce your risk of heart attacks and strokes in those with high cholesterol.
Common statins include:
- Zocor (simvastatin)
- Lipitor (atorvastatin)
- Crestor (rosuvastatin)
- Lescol XL (fluvastatin)
- Altoprev (lovastatin)
- Livalo (pitavastatin)
- Pravachol (pravastatin)
Muscle aches and brain fog are common side effects. For many years, researchers didn’t understand why some people who took statins had muscle aches and even severe weakness, but they’ve recently learned that it may be because they interfere with an important enzyme. People with genetic mutations in this enzyme can develop a rare, but devastating type of muscular dystrophy. Rarely, some patients have experienced liver damage, severe muscle damage, or an increased risk of diabetes. There’s debate among experts about who benefits most from the drugs and whether they’re overprescribed.
Nexletol and Nexlizet are both recently-approved drugs that can be prescribed if using a statin alone hasn’t sufficiently lowered your cholesterol
Drugs that Can Raise Your Risk for Heart Disease
A lot of drugs for unrelated conditions can raise or lower your blood pressure as one of its side effects. Some of those drugs include:
DrugsThat Can Raise Blood Pressure:
- Decongestants
- Caffeine
- Corticosteroids
- NSAIDS
- Oral contraceptives
- Serotonin norepinephrine reuptake inhibitors (SNRIs)
Drugs That Can Lower Blood Pressure:
- Diuretics
- Opioids
- Drugs for Parkinson’s disease, such as Mirapex (pramipexole) or those containing L-Dopa (levodopa)
Drugs That Can Either Raise or Lower Blood Pressure
- Alcohol
- Monoamine oxidase inhibitors (MAOIs) for depression
- Selective serotonin reuptake inhibitors (SSRIs)
What Are the Signs of Heart Disease from Drugs?
Treatments for cancer, such as chemo and radiation, can raise your risk for heart failure. The signs of heart disease from drugs are the same as signs of heart disease from any other cause. You may feel fatigued, short of breath, swelling in your hands or feet or dizziness.
If you’ve been prescribed certain drugs known to cause heart disease, such as chemotherapy, your healthcare providers should be monitoring your heart function regularly.
Questions to Ask Your Doctor About Your Heart Medicines
Depending on your condition, the chance that your doctor will prescribe a new medication is likely. Given the serious nature of these diseases, intervention is often required.
Even when medicines are the only answer that may help, you still will want to be clear with your healthcare provider to be sure that you understand your medications, their risks, and potential side effects.
Some questions to ask your doctor include:
- How does this drug work?
- Why do I need this medicine?
- How long will I need to take it?
- Are there any alternatives I should consider?
- What are the most common side effects?
- Are there any dangerous side effects?
- Are there any risks that are specific to me, for example because of my gender or other factors?
- What might interact with this medicine? Be sure to ask about other prescription drugs, over the counter drugs, supplements, and even foods.
- If I have a cold, are there cold medicines I need to avoid?
- What else can I do to help reduce my risk of heart attacks or strokes?
Infographic: How to Spot a Heart Attack






