Prilosec, Acid Reflux Drug
When Rocky Angelucci first went on Prilosec for his acid reflux, he considered it “a miracle drug,” wiping out his sore throat and other symptoms. But over the next decade, whenever he tried to go off the acid reflux drugs, he’d feel even worse than before he started taking it.
“I felt horrible burning, choking reflux,” says Angelucci, 53, a technical writer and author in Texas. “It felt like I had swallowed a potato and it was stuck halfway down, along with burning acidity.”
Angelucci finally was able to quit Prilosec (omeprazole) — one of the most popular over-the-counter (OTC) drugs for acid reflux — for good eight years ago. What made the difference? First, he radically changed his diet, cutting refined grains, white sugar and processed foods. Second, to get through the rebound reflux stage, he used herbal remedies, including licorice chews and apple cider vinegar.
Now, he says, reflux is “a distant memory.”
Side Effects Associated With Long-Term PPI Use
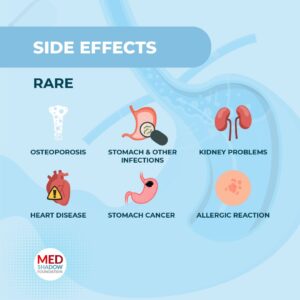
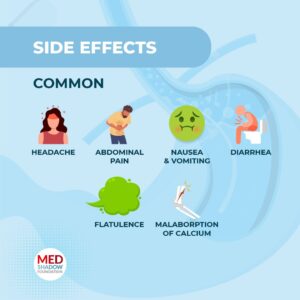 Millions of Americans take medications such as Prilosec and Nexium (esomeprazole) – which are proton pump inhibitors (PPIs) that work by suppressing stomach acid. Sometimes acid reflux progresses to gastroesophageal reflux disease (GERD), a more severe form of reflux. People who develop GERD may need to take PPIs for longer periods. And some people take these acid reflux drugs long term due to a precancerous condition called Barrett’s esophagus, which can develop if GERD continues unchecked. But long-term use of PPIs has been associated in recent years with conditions such as osteoporosis, stomach and other infections, kidney problems, and heart disease, stomach cancer, and possibly an increased risk of contracting COVID-19. Some research even suggests an increased risk of death with long-term PPI use.
Millions of Americans take medications such as Prilosec and Nexium (esomeprazole) – which are proton pump inhibitors (PPIs) that work by suppressing stomach acid. Sometimes acid reflux progresses to gastroesophageal reflux disease (GERD), a more severe form of reflux. People who develop GERD may need to take PPIs for longer periods. And some people take these acid reflux drugs long term due to a precancerous condition called Barrett’s esophagus, which can develop if GERD continues unchecked. But long-term use of PPIs has been associated in recent years with conditions such as osteoporosis, stomach and other infections, kidney problems, and heart disease, stomach cancer, and possibly an increased risk of contracting COVID-19. Some research even suggests an increased risk of death with long-term PPI use.
 Research shows that most people who take PPIs are concerned about the side effects, and many will attempt to discontinue their use. But many who want to try getting off PPIs often find that rebound hyperacidity makes this challenging. A 2006 study showed only 27% of long-term users who tried to stop PPIs were successful. In a more recent study of patients on long-term PPI treatment who were given a placebo or Nexium also found that just over a quarter of patients in the placebo arm were able to discontinue PPI treatment.
Research shows that most people who take PPIs are concerned about the side effects, and many will attempt to discontinue their use. But many who want to try getting off PPIs often find that rebound hyperacidity makes this challenging. A 2006 study showed only 27% of long-term users who tried to stop PPIs were successful. In a more recent study of patients on long-term PPI treatment who were given a placebo or Nexium also found that just over a quarter of patients in the placebo arm were able to discontinue PPI treatment.
One way PPI users may more easily wean off the acid reflux drugs is to use herbal medicine, say integrative medicine specialists.
“Herbs and supplements have some mechanisms of action on the esophagus and stomach that’s a little different than pharmaceuticals,” says David Kiefer, MD, a family physician trained in integrative medicine and clinical assistant professor at the University of Wisconsin-Madison department of family medicine and community health.
Herbs Ease Inflammation, Coat Tissue on GI Tract
Some herbs can ease inflammation on the surface of the gastrointestinal (GI) tract, Kiefer says. These anti-inflammatory herbs include chamomile tea and licorice root (specifically, the deglycyrrhizinated type, also referred to as DGL).
Other herbs work to coat the tissue in the esophagus and stomach, Kiefer says. These include slippery elm root bark and marshmallow root, which come in powdered form that can be mixed with water. “They make kind of a slurry which goes down and coats whatever it touches — the back of your throat, your esophagus, your stomach,” says Kiefer.
Another coating type of herb, says Kiefer, is aloe vera gel — the type formulated for upper GI tract problems, not the kind you get in a bottle in your store’s sunburn section.
Besides these herbs, Kiefer recommends melatonin, which studies have found may be as effective as Prilosec at reducing GERD symptoms.
David Rakel, MD, professor and chair of the department of family and community medicine at the University of New Mexico, adds Iberogast to the list of natural products that can help people get off PPIs. Iberogast is the brand name of a compound comprised of 9 herbal extracts; studies show it’s effective in relieving gastric regurgitation and other symptoms.
How to Use Herbals to Transition Off PPIs?
Rakel says the key is to set expectations. “I say, ‘Hey, this is one of those things where you’re going to get worse before you’ll feel better, but if you can hang in there for 1 1/2 to two weeks, that hyperacidity rebound effect should go away.’”
Rakel says it’s important for patients to taper off PPIs slowly, first cutting the dose, if possible, and then taking it every other day. He usually recommends patients stay with one herbal remedy while weaning off PPIs.
Kiefer, on the other hand, says patients can combine herbs. He suggests using anti-inflammatories such as chamomile or DGL plus melatonin during the medication tapering process. Once the PPI is gone, herbs that act to coat the GI tract (such as aloe vera or marshmallow root) can be added, he says. (These can interfere with the absorption of medication, so should be taken at least an hour before or after taking any pills.)
Becky Fishman used a process like this to finally get off PPIs after a dozen years. She says her doctor hadn’t explained how, but her father — also a reflux sufferer — helped her work out a Nexium step-down plan. The 46-year-old North Carolina medical writer used DGL lozenges and aloe vera to help alleviate symptoms during her transition. Some mild reflux symptoms remained, though, which she then mostly eliminated by cutting back on carbs.

Indeed, say Rakel and Kiefer, changing what you eat can also help avoid reflux symptoms, whether it’s avoiding trigger foods or eating less. Other non-herbal remedies they advise include acupuncture, stress management (mindfulness and meditation, for instance) and lifestyle changes, such as exercising and losing weight.
What If Acid Reflux Symptoms Return?
If you are off your medication for a few weeks and your reflux symptoms have come burning back, Rakel and Kiefer say patients should be evaluated to see why. Some patients may have hiatal hernias or precancerous changes to the esophagus (Barrett’s esophagus), for example, which may mean they need to go back on acid-blocking medication or explore other treatments.
What Kiefer and Rakel won’t do is recommend you stay on a regular regimen of herbs to fight reflux. If you have occasional mild heartburn, you can take an herbal remedy, they say, but if your problem is severe and ongoing, you want to find out what the cause is — not just mask its symptoms.
“I would be doing a disservice if I just swapped out a drug for an herb,” says Kiefer.
Angelucci says he decided to go off his PPI because he didn’t want to be on a drug for the rest of his life; he wanted to see if he could address the reason for his symptoms. In his case, it turned out to be his diet, he says.
In fact some research suggests that starting with a change in diet may be more effective than PPIs in reducing acid reflux symptoms. According to a study published in JAMA Otolaryngology-Head & Neck Surgery, people with laryngopharyngeal reflux — when acid travels up the esophagus to reach the throat — were divided into two groups. More than 60% of those in the group that closely followed a Mediterranean diet saw improvement in reflux symptoms compared to only 54% who in the group that took PPIs.
The Mediterranean diet is plant and whole foods-based and focuses on eating fruits, vegetables, grains and nuts. Dairy and animal products are largely cut out, as are the refined grains and processed foods that Angelucci ditched from his diet.
The study’s lead author, Craig H. Zalvan, MD, medical director of The Institute for Voice and Swallowing Disorders at Phelps Hospital in Sleepy Hollow, NY, used to be one of the biggest prescribers of PPIs in the area. But he thought there had to be a better treatment for reflux and through research, developed a plant-based diet for some of his patients.
“Although effective in some patients, I felt acid reflux drugs couldn’t be the only method to treat reflux and recent studies reporting increased rates of stroke and heart attack, dementia and kidney damage from prolonged PPI use made me more certain,” Zalvan said in a statement. “The results we found show we are heading in the right direction to treating reflux without medication.”
“My diet was the root cause of my reflux symptoms,” Angelucci says. “But the herbal supplements were a dramatic help during that really difficult roller-coaster period.”






